Making Connections
D. James Surmeier, PhD, has steered the Department of Neuroscience to a new name and growing recognition of Northwestern Medicine’s prominence in neuroscience research.
by Cheryl SooHoo
Photography by Teresa Crawford
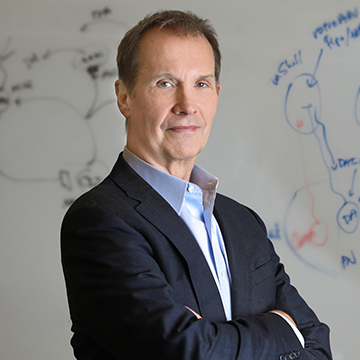
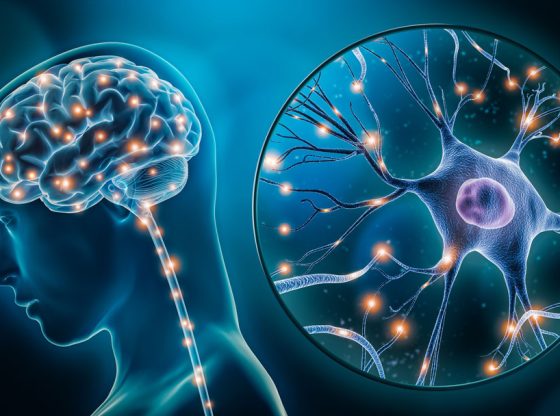
What’s in a name? Plenty, says D. James Surmeier, PhD, chair of the recently renamed Department of Neuroscience, formerly known as the Department of Physiology. The name was officially changed in September to better reflect Northwestern Medicine’s exceptional strength in neuroscience. But long before the new departmental letterhead landed on his desk, Surmeier, who has been chair since 2001, had already begun the work of bringing the academic unit national and international attention.
“In the last 20 years, we have built a critical mass of talent in neuroscience, doubling our size by recruiting the best and brightest young neuroscientists. At Feinberg, we now have one of the largest neuroscience groups in the country. The research being done here is at the cutting edge in many areas of neuroscience, including movement control, neurodegenerative disorders, and neuropsychiatric disorders. It’s also a great place for young neuroscientists to come and train — to find their bliss. The name change recognizes what we aspired to be and have become,” says Surmeier, who is also the Nathan Smith Davis Professor of Neuroscience.
“As a department of physiology, we were consistently ranked in the top 5 to 10 programs in the country,” he adds. “Although the pool of neuroscience departments is deeper, if the rankings were to be done today, we’d be in the top 10 in the nation.”
Building Bridges Across the University
The designation of neuroscience more appropriately describes what the department has been doing for decades: piloting innovative studies in how the central nervous system works — and, more importantly, when it doesn’t work and leads to neurological, psychiatric, and neurodevelopmental disorders.
Investigators focus on topics that span molecular, cellular, systems, and behavioral levels. Basic studies range from single-channel recording to behavioral analysis. Translational work in the department’s research portfolio includes Parkinson’s disease (PD), Alzheimer’s disease, Huntington’s disease, epilepsy, autism, schizophrenia, brain-machine interfaces, and chronic pain.
“But, of course, at Northwestern, the study of neuroscience is much broader than our department,” says Surmeier.
The collaborative environment here at Northwestern is second to none.
D. JAMES SURMEIER, PHD
The discipline draws upon expertise in myriad fields across the university’s two campuses, ranging from chemistry, engineering, computer science, and biology to areas within the medical school, including neurology, neurosurgery, anesthesiology, psychiatry and behavioral sciences, and pharmacology.
“One of our aims will be to build bridges that foster scientific dialogue, cooperation, and collaboration,” Surmeier says. “With the new name, we will build upon our achievements and serve as a beacon to the outside world that there is great neuroscience being conducted at Feinberg and Northwestern at large.” A flurry of requests has already come from faculty members seeking secondary appointments. “The collaborative environment here at Northwestern is second to none,” Surmeier says.
Steady Growth, Collaborative Discovery
In the late 1970s, while pursuing a PhD degree in mathematics, Surmeier became fascinated with how the brain functions — in particular, the basal ganglia, the part of the brain that controls movement. The young scholar decided to shift gears and, in 1983, completed a doctoral program in physiology-psychology at the University of Washington. He has never looked back.
Joining Northwestern in 1998, Surmeier has had a prolific career in basal ganglia research, focusing on how it contributes to PD, Huntington’s disease, and chronic pain. He has authored well over 200 peer-reviewed publications, many in high-impact journals such as Science, Nature, Neuron, and Nature Neuroscience.
In the early 2000s, he and his colleagues made an exciting discovery while exploring the causes of PD. They identified a protein, or more specifically, a calcium channel that triggered mitochondrial oxidant stress in at-risk neurons. This novel finding published in Nature came as a result of collaborating with Paul Schumacker, PhD, professor of Pediatrics, Cell and Developmental Biology, and of Medicine, whose studies focus on the role of mitochondrial signaling in the development of pulmonary hypertension.
“It turned out that there were drugs approved to treat high blood pressure called dihydropyridines that inhibited this particular calcium channel,” says Surmeier. “We thought this class of drugs might help slow the progression of early-stage Parkinson’s disease.”
Subsequently, epidemiological studies revealed that patients taking these hypertension medications had a lower risk of developing PD. Surmeier partnered with clinical colleague Tanya Simuni, MD, director of the Parkinson’s Disease and Movement Disorders Center at Feinberg and the Arthur C. Nielsen Professor of Neurology. The Surmeier team’s discovery led to a phase II and then a multi-center phase III clinical trial evaluating the dihydropyridine isradipine. Ultimately, the phase III clinical trial, which was completed in 2018, failed to reach their clinical goals.
The Surmeier and Schumacker labs have continued to tease out how their target protein interacts with the mitochondria and leads to Parkinson’s disease.
One of the possible reasons why the clinical trial failed was that the cardiovascular side-effects of isradipine significantly limited how much patients could take. Knowing this limitation, Surmeier teamed with Richard Silverman, PhD, professor in the Department of Chemistry, to develop a new, more selective inhibitor of the calcium channel implicated in PD. This long-standing collaboration has led to the identification of a novel drug class that has great promise. A collaborative effort between Surmeier, Silverman, and Alfred George, MD, chair of the Department of Pharmacology and the Alfred Newton Richards Professor of Pharmacology, has recently been endorsed by the Michael J. Fox Foundation with a multi-year award to identify compounds that have clinical potential.
“We are still confident that we have the right target and that by improving delivery of isradipine to the brain or by developing a more selective inhibitor, we can slow the progression of Parkinson’s disease,” says Surmeier. “But even if achieving adequate target engagement isn’t feasible, this translational effort will teach us something important about the disease and bring us closer to a therapy that will succeed. It also has illustrated that Northwestern offers an environment that brings together people from different disciplines to effectively work toward a shared vision.”

The Surmeier and Schumacker labs have continued to tease out how their target protein interacts with the mitochondria and leads to PD. Better understanding the connection may allow for potentially changing the dialog between the two and altering the course of disease development. In a recent study published in Nature, Surmeier and Schumacker demonstrated that loss of mitochondrial complex I function in dopaminergic neurons is sufficient in mice to produce a progressive, levodopa-responsive parkinsonism with features that closely resemble those of human PD. This work establishes a clear chain of events – from calcium channel mediated over-stimulation of mitochondria, to mitochondrial oxidant stress and damage to complex I, to PD pathogenesis.
As is often the case in science, there were unexpected findings, according to Surmeier. In this case, the progressive nature of the model allowed the investigators to dissect the role of regional dopamine depletion in driving PD symptoms. This work led to the surprising conclusion that the output of the basal ganglia (the substantia nigra) was a critical site of dopamine action in preventing movement deficits. Surmeier’s team then demonstrated that a gene therapy could significantly boost the effects of levodopa in a model of late-stage PD — providing a potential alternative to deep brain stimulation.



Novel Research Findings
Undeniably excited about asking research questions and finding the answers to them, Surmeier’s curiosity has continued to yield novel research discoveries with translational implications.
One long-standing mystery has been why neurons that release dopamine are particularly vulnerable in PD. A collaborative study with Dimitri Krainc, MD, PhD, chair and Aaron Montgomery Ward Professor of Neurology, published in Science a few years ago, revealed that this vulnerability could be traced to an interaction between mitochondria and dopamine. But the precise nature of this interaction was unclear.
Teaming with Krainc and Schumacker, Surmeier and his associates discovered that mitochondria were metabolizing dopamine in axons — the most at-risk part of the neuron — to help them generate energy (adenosine triphosphate) for transmitter release. This boosting was mediated by monoamine oxidase (MAO) tethered to the outer membranes of the mitochondria. This process created oxidant stress on the mitochondria, particularly when dopamine synthesis was boosted by a precursor of dopamine — levodopa. This new finding has provided more insight into the role mitochondria, dopamine, and MAO play in PD and how that knowledge can inform current and future treatment. Patients with early-stage PD, for example, are often given MAO inhibitors to help boost dopamine levels in the brain. Published in Nature Neuroscience, this study suggests that this treatment strategy protects vulnerable dopaminergic neurons by limiting mitochondrial stress and damage.
Connecting seemingly disparate “dots” often leads to breakthroughs in science. A key feature of PD pathology is the formation of intracellular aggregates of a protein called alpha-synuclein. It has been thought that these aggregates spread through the brain, much like a prion. In a study published in Science Advances in 2020, Surmeier’s team showed that strength or number of neuron-to-neuron connections was not a good predictor of how alpha-synuclein pathology spread. This finding raised the possibility that other neuronal traits, like mitochondrial oxidant stress, were important factors. The Northwestern investigators are actively pursuing the mitochondrial connection and exploring possible links between pathogenic mechanisms in PD. This work opens the door to the potential use and effectiveness of combination therapies to slow disease progression.
In another area of research, Surmeier has made inroads in developing the first viable treatment for Huntington’s disease — a degenerative disease characterized by progressive motor and cognitive impairment and caused by alteration in the “huntingtin”gene. His team has published a series of papers in journals such as Nature Medicine, demonstrating that lowering mutant huntingtin with a zinc finger gene therapy effectively reverses neuronal pathology and behavioral deficits in animal models of Huntington’s disease.
“We have an extraordinary opportunity to better understand the brain and to develop new treatments for brain disorders,” he says. “New technologies are allowing us to link brain function at the molecular, cellular, and circuit levels to behavior in unprecedented ways. At the same time, we have a growing set of tools for correcting neuronal dysfunction that is making its way into the clinic. We truly have exciting times ahead of us.”
Leading the Way
The newly named Department of Neuroscience recently made another new name for itself on the world stage. This October, the Aligning Science Across Parkinson’s (ASAP) initiative awarded not only one but two $9 million grants to two different teams of Feinberg neuroscientists exploring the biological causes of PD to develop new therapies.
“To have two of 14 successful groups in this intense international competition come from Northwestern is an extraordinary accomplishment,” says Surmeier, the coordinating lead principal investigator for one of the winning Feinberg projects. “This success is a testament to the fact that Northwestern has become an international leader in neuroscience research.”
Surmeier’s ASAP-funded project will explore the circuit dysfunction underlying motor and sleep deficits in a progressive mouse model of PD. Better understanding how this dysfunction begins could offer promise for earlier diagnosis, development of disease-modifying therapies, and enhanced treatment strategies for patients with later-stage PD. New faculty member Ann Kennedy, PhD, assistant professor of Neuroscience, and other co-investigators at Columbia University, University of California, Berkeley, and the University of Basel (Switzerland) will be serving as co-investigators.
An ASAP award also went to Rajeshwar Awatramani, PhD, professor of Neurology in the Division of Movement Disorders, and his team for their project entitled “Redefining PD Pathophysiology Mechanisms in the Context of Heterogeneous Substantia Nigra Neuron Subtypes.” This project involves neuroscience faculty from Feinberg, as well as neurobiology faculty on the Evanston campus.
Launched in 2017, the ASAP initiative is a private organization of funders working with the Michael J. Fox Foundation for Parkinson’s Research to accelerate discovery by building a collaborative research network. PD is one of the most common movement disorders in the world, with some six million people living with the disease.
This most recent competition called for applications that focused primarily on circuitry and brain-body interactions — both areas of expertise at Northwestern.
“These awards reflect the commitment of Northwestern to excellence in neuroscience research across both campuses,” Surmeier says.