by EMILY AYSHFORD
To better understand sleep and its implications in health, Northwestern investigators look to circadian rhythms.
Sleep has become a critical topic, with one main message: Most people don’t get enough of it. In fact, Northwestern research has shown just how detrimental our disrupted sleep and biological rhythms can be for health and productivity.
When we sleep, our blood pressure drops, our tissue is repaired, and our memories are consolidated and stored. But what regulates this is not sleep itself, but the body’s circadian rhythms — the roughly 24-hour cycle every being lives on.
When those rhythms are disrupted, it can affect everything from learning and memory to metabolic and cardiovascular diseases. Feinberg investigators are both undertaking basic science research to understand the implications and turning that information into translational medicine for patients, including new medicines, interventions, and strategies aimed at improving not just sleep, but overall health.
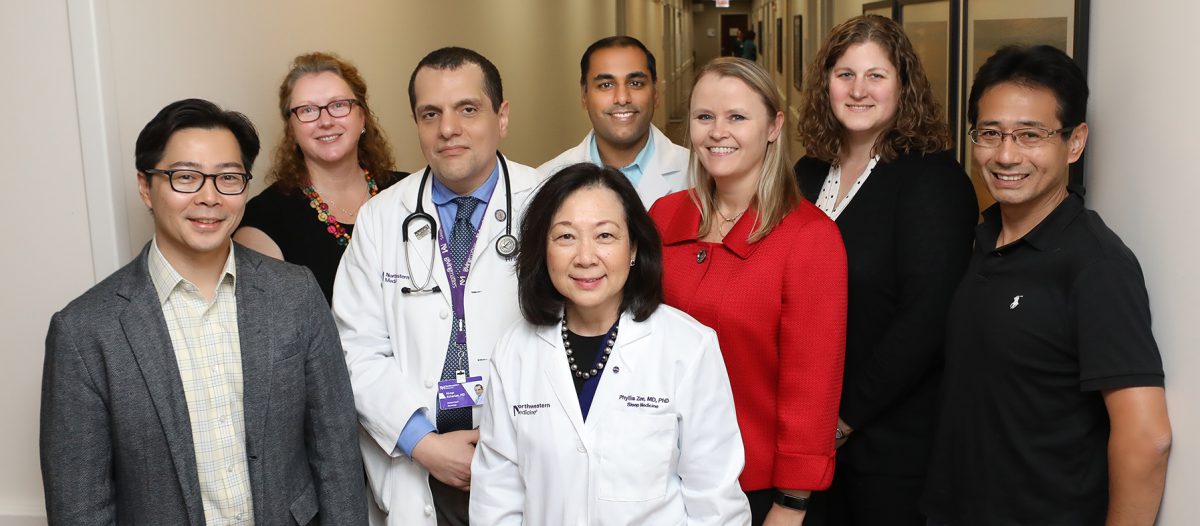
“Circadian rhythms and sleep affect the function of all cells,” says Phyllis Zee, MD, PhD, the Benjamin and Virginia T. Boshes Professor of Neurology and director of the Center for Circadian and Sleep Medicine. “We’re at an exciting time when we are beginning to understand just how integrally involved sleep and circadian clocks are with both promoting health and resilience and, when disrupted, increasing the risk for disease.”
Night owl or morning lark? It could affect your health.
When you become sleepy in the evening, you can thank your body’s network of clocks. The brain’s master circadian clock, located in the suprachiasmatic nucleus of the hypothalamus, was once thought to control the circadian rhythm across all the body’s peripheral clocks, which are located in nearly every cell and organ in the body.
But the story is more complicated. These clocks — regulated by genes and affected by environmental cues, such as light — work together like an orchestra to regulate not only sleep, but other behavioral and biological processes, including hormone release and eating habits.
That doesn’t mean every human runs on the same circadian clock: Scientists have dubbed those who rise early as “morning larks,” while those who prefer to stay up late are “night owls.”
Whether you are a morning lark or night owl depends equally on both genetic and environmental factors, but research shows that it could affect your health.
In a study of nearly half a million participants in the U.K. Biobank Study, Feinberg investigators found that night owls have a 10 percent higher risk of dying than larks over the 6 ½ years of the study. The results were published in Chronobiology International.
“It could be that people who are up late have an internal biological clock that doesn’t match their external environment,” says co-lead author Kristen Knutson, PhD, associate professor of Neurology. “It could be psychological stress, eating at the wrong time for their body, not exercising enough, not sleeping enough, being awake at night by yourself, maybe drug or alcohol use. There are a whole variety of unhealthy behaviors related to being up late in the dark by yourself.”

Racial disparities in sleep could lead to higher risk for disease
While living according to an external clock that doesn’t match the internal clock can result in increased mortality, so can reduced sleep due to elevated exposure to social stress, like discrimination.
That was the finding from a Feinberg study published in the Proceedings of the National Academy of Sciences that found that African-Americans got 40 fewer minutes of sleep per night compared to European-Americans, and had a 10 percent lower sleep efficiency rate. Poor sleep patterns could explain, in part, the differences in the risk of cardiometabolic disease, said study author Mercedes Carnethon, PhD, professor of Preventive Medicine in the Division of Epidemiology.
African-Americans have higher rates of cardiovascular disease, stroke, diabetes, and hypertension than European Americans, even when controlling for health behaviors. By studying the sleep patterns of 426 African-American and European-American adults who were included in the Midlife in the United States (MIDUS) study, the investigators found that more than one half of racial disparities in cardiometabolic risk could be explained by sleep disparities.
“This study is one of the first to examine how disparities in sleep are contributing to differences in metabolic diseases,” Carnethon says. “What we hope is that as patients and healthcare providers become aware of these associations, they will prioritize considering sleep as an essential component of a healthy lifestyle.”
Measuring Time In and Out of Our Bodies
Phyllis Zee’s office is a monument to time. A Dali clock drips from a bookshelf. An hourglass sifts sand on the table. A kinetic clock sculpture circles chaotically on her desk. Timing is everything, she always says, and the saying may be true in medicine, as well. Zee and her collaborators have developed the first simple blood test to identify your body’s precise internal time clock as compared to the external time.
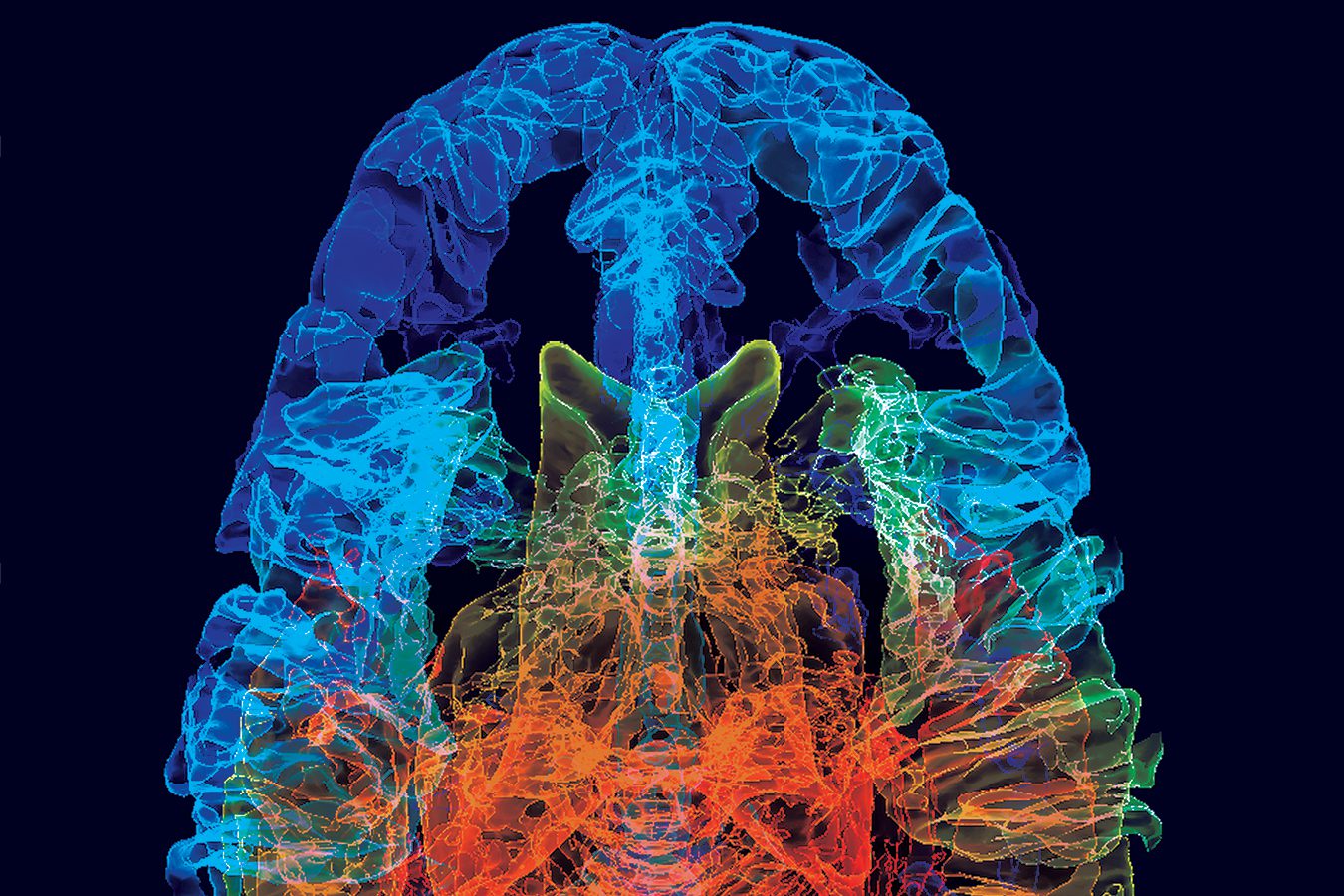
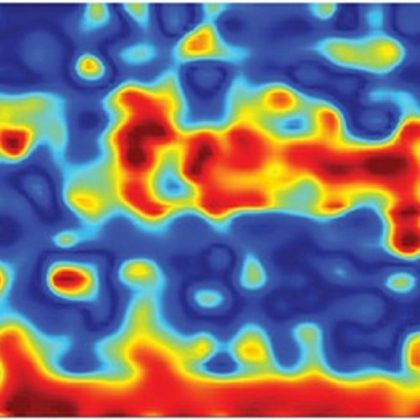
Called TimeSignature, the test requires two blood draws and measures 40 different gene expression markers to determine the “time” inside your body. Your body might think it’s 10 a.m., for example, when it’s really 6 a.m. The investigators — including Rosemary Braun, PhD, MPH, assistant professor of Preventive Medicine in the Division of Biostatistics, as well as Sabra Abbott, MD, PhD, assistant professor of Neurology, and Ravi Allada, MD, professor of Neurobiology — published their results in the Proceedings of the National Academy of Sciences.
The test can potentially help physicians and investigators to tell the time of one’s internal biological clock and determine if circadian rhythms are misaligned. It can also help them consider when to provide doses of medication. New research indicates medicine might be more effective at different times of day, depending on the timing of a person’s circadian rhythms.
How diabetes and obesity are linked to circadian rhythm
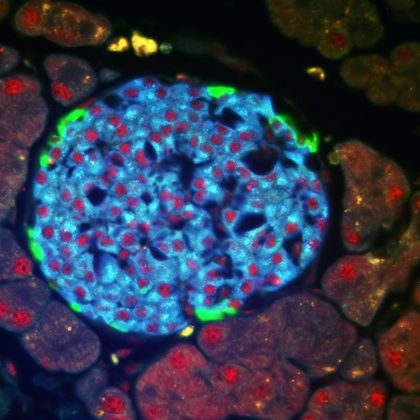
Understanding just what role circadian rhythms play in metabolic disorders like obesity and diabetes is the goal of Joe Bass, MD, PhD, chief of Endocrinology, Metabolism and Molecular Medicine in the Department of Medicine.
In 2005, Bass and his collaborators published a study in Science that showed that a misaligned biological clock impaired metabolism, increasing obesity. Since then, Bass has studied how these clocks regulate feeding behavior and glucose metabolism. In 2010, he found that beta-cells in the pancreas require a clock to produce insulin and published the research in Nature, and in 2015, he found the precise set of genes in the pancreas that are controlled by the clock transcription factors. Those findings were published in Science.
Bass and Zee are studying how nighttime fasting affects circadian rhythms. “We will look at the peripheral clocks in the body to see how controlled, restricted feeding affects metabolic aging,” Bass says. Other collaborators on the study include Knutson and Kathryn Reid, PhD, research professor of Neurology.
“We think that by not eating for 12 hours or more at night, people will have an enhanced metabolic rhythm, which could have positive effects on conditions like obesity,” Zee says.
Medicine and sound stimulation for a better night’s sleep
In the Center for Circadian and Sleep Medicine, Zee and her collaborators are developing new strategies to help people get more — and better — sleep.
In 2017, they found that a synthetic cannabis-like drug in a pill could be effective in treating obstructive sleep apnea, a sleep disorder in which a person stops or has shallow breathing for 10 seconds or more while sleeping. Sleep apnea patients are at increased risk for heart disease, diabetes, sleepiness, and cognitive impairment. The usual and most effective treatment for the disease is CPAP (Continuous Positive Airway Pressure), a device that delivers pressurized air to open up the airway, but compliance can be poor.
The drug, dronabinol, is a synthetic version of the molecule Delta-9 THC (tetrahydrocannabinol), which is in cannabis. It was originally approved by the Food and Drug Administration to treat nausea and vomiting in chemotherapy patients.
“The drug targets the brain and nerves that regulate the upper airway muscles,” says Zee, who is also the chief of the Division of Sleep Medicine. “It alters the neuro- transmitters from the brain that communicate with the muscles. Better understanding of this will help us develop more effective and personalized treatments for sleep apnea.”
Some strategies don’t involve drugs at all — instead, they involve just the right noise.
In a study done by Zee, Reid, Roneil Malkani, MD, assistant professor of Neurology in the Division of Sleep Medicine, and Daniela Grimaldi, MD, PhD, research assistant professor of Neurology in the Division of Sleep Medicine, people with mild cognitive impairment found enhanced deep sleep through the use of “pink noise” — gentle sound stimulation at a certain frequency played during specific times of deep sleep.
Because the brain records sound while you sleep — potentially eavesdropping for dangers — the sound could provide a signal to the brain that everything is okay, and that it should protect you while you are in deep sleep, which is important for memory consolidation.
The noise even worked on healthy older people, improving memory by up to 30 percent. “It’s all a race against time,” Zee says. “If we can find strategies that enhance sleep quality, the hope is that maybe we can delay cognitive impairment and improve cardiovascular and metabolic functions for successful aging.”
A mindful approach to sleep
For Jason Ong, PhD, associate professor of Neurology, getting a good night’s sleep involves not only behavioral changes, but a whole new mindset.
That’s why Ong has encouraged insomnia patients to take a mindfulness-based approach to sleep. Many approaches to falling asleep involve standard behavioral changes — get out of bed if you can’t sleep, spend less time in your bed overall. But Ong found that many patients don’t like to follow such rules, so he developed a mindfulness-based intervention.
By learning how to meditate — how to objectively look at thoughts, but let them continue on, like trains traveling past a station — those with insomnia who participated in a small trial showed improvements not only in sleep but in their daytime moods.
“It’s not about hypnotizing yourself to sleep,” says Ong, who is also a professor of Medical Social Sciences and Psychiatry and Behavioral Sciences. “It’s about being present in the moment and understanding that maybe you don’t need to be in bed, or maybe you don’t need as much sleep tonight. It cultivates awareness about whether you are truly sleepy. When people are aware, it can help remove the stress of insomnia.”
Such work underscores the role of sleep on nearly every aspect of health, Zee says. That’s why the last decade, when investigators began to understand how circadian rhythms affect the body, has laid the groundwork for an exciting future in the field.
“Circadian rhythms work together like a beautiful orchestra, or jazz band,” Zee says. “We are just beginning to understand how these rhythms underlie so many diseases, and we’re ready to translate that knowledge into real treatments.”
Strategies for Getting the Best Sleep
Research has shown that it’s not how much sleep you get — it’s when you go to sleep and wake up that matters. Below, a few tips from Northwestern investigators:
1. Stop eating two to three hours before going to sleep.
2. Two hours before going to sleep, dim the lights.
3. Before going to bed, take a bath. This dissipates heat from your body and signals that it’s time to sleep.
4. Go to bed at the same time every night. If this isn’t possible, keep it within a one-hour window during the week, and a two-hour window on the weekends.
5. Get up at the same time every morning, also ideally within a one-hour window.
6. When you get up, seek out daylight to help tune your circadian rhythms.
7. Exercise, ideally at the same time every day (or however often you exercise).