Modern Malady
Feinberg investigators are finding
new ways to tackle metabolic syndrome.
by Emily Ayshford
One of the biggest diseases of the modern era is a pernicious cluster of risk factors called metabolic syndrome that together raise the risk for heart disease, stroke, and Type 2 diabetes. About one in three adults in the United States has metabolic syndrome, and the number keeps climbing.
“Metabolic syndrome is highly over-represented in our population,” said Douglas Vaughan, MD, chair and the Irving S. Cutter Professor of Medicine. “It’s mostly related to the epidemic of obesity in our country.”
In addition, the syndrome is linked to lack of physical activity and insulin resistance — which could potentially be controlled with lifestyle changes. But other factors, particularly aging, and situations when lifestyle changes aren’t an option, remain an open challenge for physicians and investigators.
Northwestern scientists across disciplines are looking for new ways to understand, target, treat, and even prevent this syndrome, with the hopes of ultimately creating a much healthier nation. The good news is they are making progress.
“We are all interested in developing new ideas on how to treat it and prevent it,” says Vaughan. “And it’s incredibly exciting and gratifying that we are now at the point where we could potentially do that and help a large part of the population.”
Metabolic syndrome is highly over-represented in our population. It’s mostly related to the epidemic of obesity in our country.
Douglas Vaughan, MD, chair and the Irving S. Cutter Professor of Medicine

PREVENTING THE DEVELOPMENT OF METABOLIC SYNDROME
To be diagnosed with metabolic syndrome, a patient must have three of five risk factors: a large waistline, a high triglyceride level, a low HDL cholesterol level, high blood pressure, and high fasting blood sugar levels.
Investigators have found a potentially wide-ranging therapeutic target that could affect all of them. Plasminogen activator inhibitor 1 (PAI-1), a protein found in the blood, has been shown to be an important driver of several components of metabolic syndrome, including obesity, high blood pressure, and insulin resistance.
In a recent study published in Scientific Reports and led by Vaughan, Feinberg investigators administered a new drug that blocks the activity of the PAI-1 in a mouse model. The team used RNA sequencing and gene expression analysis techniques to analyze liver mRNA in mouse models of metabolic syndrome. They found that the PAI-1 inhibitor drug regulated liver lipid metabolism by reducing the expression of PCSK9 and increasing the expression of FGF21. Notably, drugs that block the production or function of PCSK9 are effective in reducing cardiovascular disease, and there is increased interest in developing FGF21-targeting drugs to prevent and treat obesity-related metabolic complications.
“Here’s one singular factor that we could potentially target, and by doing so, prevent metabolic syndrome itself, as well as the cardiovascular morbidity and mortality that’s associated with the syndrome,” said Vaughan, who led the research.
The current findings build off previous work from the Vaughan laboratory involving a Swiss Amish community in Indiana with a mutation in the gene that codes for PAI-1. There, they have found that lower levels of the protein protected against the development of diabetes, improved insulin sensitivity, and protected against the biological manifestations of aging.
Vaughan and his collaborators are working with a biotech company in Japan, which has developed a small molecule PAI-1 blocker, and now have FDA approval to begin testing the drug in high-risk COVID-19 patients at Northwestern Medicine, with the hopes of eventually getting approval to use it to treat patients with metabolic syndrome.
A NEW APPROACH TO TREATING OBESITY
Perhaps the single biggest factor in metabolic syndrome is obesity. If a person with obesity loses weight, the positive health effects often cascade, including lower blood pressure, better blood glucose levels, and lower triglyceride levels. But for many people, losing weight is difficult. Bariatric surgery, often the most successful intervention available, is invasive and can be prohibitively expensive. Appetite suppressants have been on the market for years, but results are mixed.
A new anti-obesity medication has been found to be almost twice as effective as current weight loss drugs, according to a new study conducted at Northwestern Medicine and published in the New England Journal of Medicine. The drug, semaglutide, is a diabetes drug, often marketed under the names Ozempic and Rybelsus. A glucagon-like peptide 1 analogue, the drug improves the body’s ability to secrete insulin and decreases appetite, which is thought to result from direct and indirect effects on the brain.
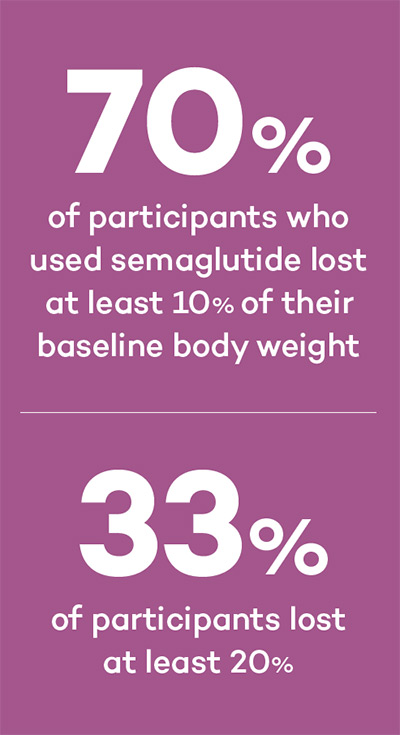
In higher doses, semaglutide has been found to be an effective appetite suppressant. In the study of nearly 2,000 adults over 68 weeks, the investigators found that 70 percent of participants lost at least 10 percent of their baseline body weight, while one third lost at least 20 percent — a weight loss thres-hold achieved through bariatric surgery for many patients.
“Not only did they lose weight, they became healthier,” said Robert Kushner, MD, ’80, ’82 GME, professor of Medicine in the Division of Endocrinology and of Medical Education, who was the corresponding author on the study. “Their blood pressure dropped, their waist circumferences went down, triglycerides came down, fasting blood sugar levels dropped, and they had less inflammation. They were much healthier metabolically.”
The drug, administered through a weekly subcutaneous injection, has been submitted for approval to the FDA for use as a weight loss treatment.
“This is the beginning of a new generation of hormonal medications that will be much more effective in treating obesity,” Kushner said. “Oftentimes when patients visit their primary care provider, obesity is on the backburner. Providers are not having conversations around this. But this drug is a way that they can have the conversation and bring obesity treatment to the front of the line.”
FINDING CLUES IN CIRCADIAN RHYTHMS
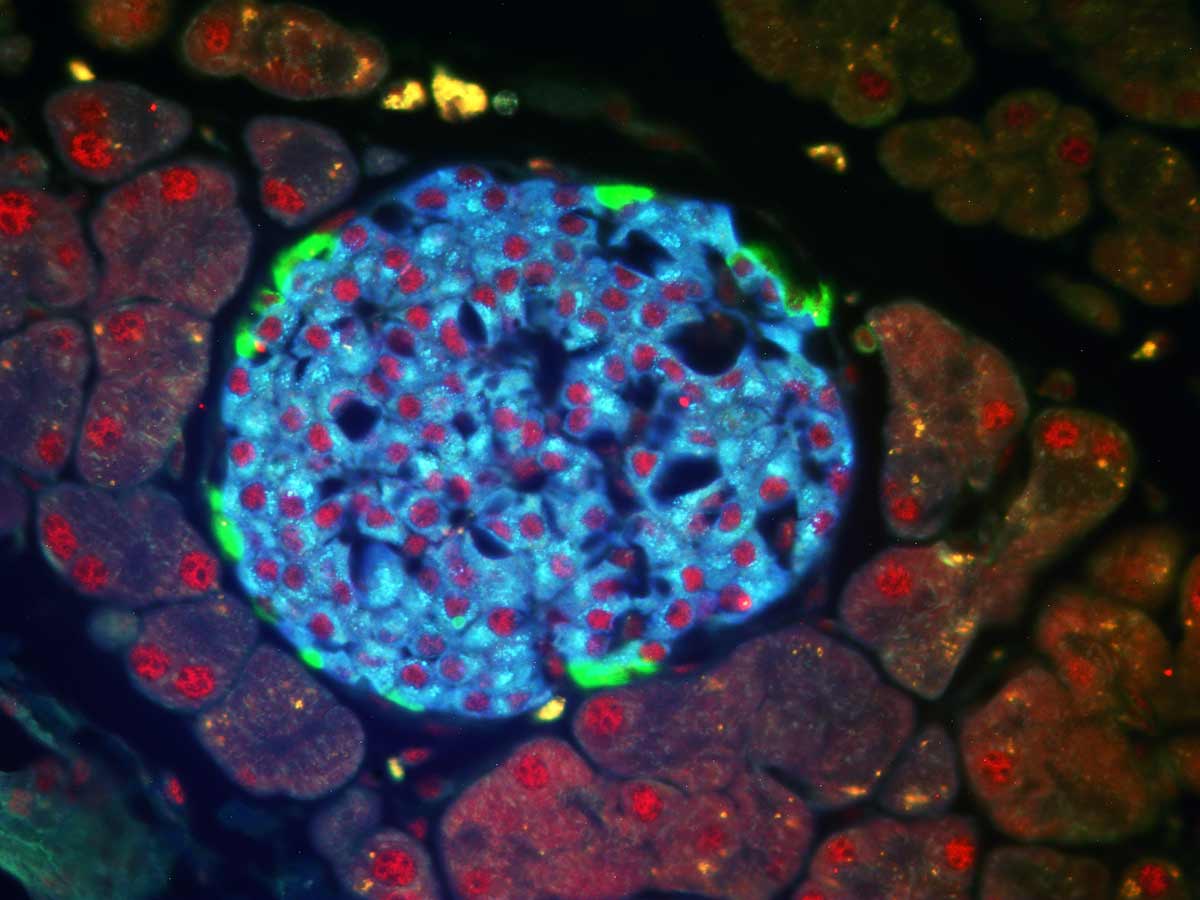
Another important aspect to preventing metabolic syndrome is controlling blood sugar levels. To better understand how the pancreas regulates insulin, Joseph Bass, MD, PhD, examined the gene transcription machinery that controls circadian rhythm.
Many years ago, Bass, the Charles F. Kettering Professor of Medicine in the Division of Endocrinology and director of the Center for Diabetes and Metabolism, discovered that turning off a gene crucial for clock transcription caused mice to develop diabetes due to lack of insulin production.
Now, in a study published in Genes and Development, Bass and his collaborators found that mouse models with a mutated clock gene also failed to release insulin from beta cells in the pancreas due to aberrant RNA splicing, a re-shuffling of RNA that occurs in gaps between coding regions. This is the first time scientists have identified RNA regulation as a mechanism by which the internal body clock affects systems beyond the sleep-wake cycle.
Mice without the clock gene had dramatically lower levels of insulin released during the time of day when animals eat, resulting in diabetes and obesity.
“Irregular sleep, shiftwork, light exposure at night, and overconsumption of calorie dense diet are all conditions that lead to deregulation of internal clocks,” Bass says.
“This work suggests that one hallmark in the metabolic syndrome involves impaired function of the body clock and clock control of insulin production.”
UNDERSTANDING A DIABETES WONDER DRUG
Those with metabolic syndrome already have help in the form of the drug metformin. Hundreds of millions of people worldwide take the drug to help maintain healthy blood glucose levels.
But investigators have also found that the drug is also anti-cancer, anti-inflammatory, and potentially anti-aging. (The anti-aging effect will be studied in the Targeting Aging with Metformin (TAME) trial that will engage 3,000 individuals between the ages of 65 and 75, including at Northwestern Medicine.)
Just how the drug works in all these different capacities remains a mystery that Navdeep Chandel, PhD, professor of Medicine in the Division of Pulmonary and Critical Care and of Biochemistry and Molecular Genetics, hopes to crack. As an expert in mitochondria, Chandel has proposed that the drug inhibits mitochondrial complex 1, which is central to energy and metabolite production in the cell.
He and his collaborators have shown this is the case in cancer, and now they’ve developed a mouse model that expresses a yeast protein that functions like mitochondrial complex 1 but that doesn’t bind to metformin. In the coming year, they will use the model to examine whether metformin’s anti-diabetic and anti-inflammatory properties are due to inhibiting mitochondrial complex 1.
If so, it will help scientists better understand how exactly the drug can help treat or prevent different diseases.
“The medicines that have made significant difference in promoting human health in the past 50 years include statins, aspirin, and metformin — all metabolic drugs,” Chandel says. “Now we know metformin might have even more potential to help a huge part of the population, and we need to understand just how it works. Not only could it help treat metabolic syndrome — it might ultimately end up that everyone over 70 takes this drug to counteract normal aging deterioration.”
THE COVID-19 CONNECTION
Multiple studies have shown that patients with metabolic syndrome have worse outcomes when diagnosed with COVID-19.
At Northwestern Medicine, investigators and physicians are studying whether drugs that treat aspects of metabolic syndromes help improve outcomes. Vaughan and his collaborators are testing whether a PAI-1 inhibitor helps improve outcomes of patients with COVID-19 — the only investigators in North America testing this.
Northwestern Medicine investigators also recently published research in the Journal of Medical Virology that indicates the drug metformin, which helps regulate blood glucose, is associated with reduced mortality from COVID-19.