Stopping a Silent Killer
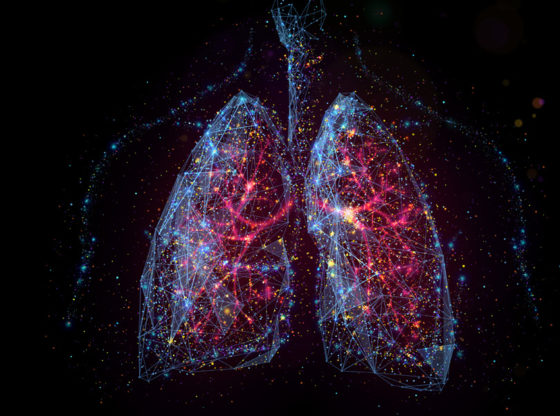
Northwestern’s unprecedented outpatient lung cancer surgery makes it safer and easier than ever for patients with early-stage disease to return to their lives — in just a few hours.
by Gina Bazer

Last spring, as COVID-19 raged and beds at Northwestern Memorial Hospital began filling up with patients fighting for their lives, thoracic surgeons found themselves in a predicament with their patients who had lung cancer.
“We didn’t have beds, and we were needing to reschedule surgeries, but we also didn’t want our patients’ cancers to spread,” recalls Ankit Bharat, MBBS, chief of Thoracic Surgery and the Harold L. and Margaret N. Method Professor of Surgery. “If left untreated, lung cancer can quickly move from stage 1 to advanced stages, and then we’ve turned a solvable problem into an unsolvable problem.”
This perfect storm called for an outside-the-box solution, and thus the Ambulatory Precision Lung Sparing (A-PLUS) surgery program was born, allowing long-awaited surgeries to take place despite the shortage of beds.

Bharat and colleagues in the Division of Thoracic Surgery and the Robert H. Lurie Comprehensive Cancer Center of Northwestern University, spent the past several years honing this highly precise, minimally invasive, lung-conserving, robot-guided outpatient surgery. Now, it is available to all Northwestern Medicine patients with a high-risk lung nodule who are referred with concerns for lung cancer. If the results of the biopsy show that the nodule is cancerous, Bharat and his colleagues are able to perform the necessary procedures to clinch the diagnosis and simultaneously treat the cancer in the Division of Thoracic Surgery in under a few hours — and on the same day, safely discharge patients who would have otherwise remained hospitalized for days.
“To be able to offer this kind of very novel therapy —that takes a deadly disease and turns it into a one-day procedure — that is the best possible scenario for our patients,” says GR Scott Budinger, MD, chief of Pulmonary and Critical Care in the Department of Medicine, the Ernest S. Bazley Professor of Airway Diseases, and professor of Medicine in the Division of Pulmonary and Critical Care.

“Innovations such as the A-PLUS surgery program continue to advance our mission to offer the most advanced and innovative care to patients with cancers within the chest cavity and position minimally invasive surgical therapies at the forefront of lung cancer treatment,” says Samuel Kim, MD, associate professor of Surgery and director of robotic thoracic surgery in the in the Division of Thoracic Surgery and of Medicine in the Division of Pulmonary and Critical Care.
Bharat, Budinger, and Kim are all members of the Lurie Cancer Center.
A team of interventional pulmonologists, surgeons — and robots
Lung cancer is the leading cause of cancer-related death in the United States among men and women, making up almost 25 percent of all cancer mortalities. This is a malignancy that tends to spread quickly, shows no symptoms unless it is very advanced, and can silently spread to virtually any part of the body. All this makes early screening and treatment critical.
To this end, Northwestern Medicine has created a fully integrated lung cancer screening and diagnosis program that works efficiently across the healthcare system. But even in a well-integrated system, between scheduling for consultations, waiting for biopsy results, and scheduling surgery, the whole process can take several weeks to months. It also incurs potentially high costs for the patient, ranging from office visits to parking fees to hotel stays for family members. The introduction of the A-PLUS program has the potential to shave off critical time to treatment, advancing patients to their next stage of treatment much faster, according to Bharat.
The first step is always a screening test for lung cancer, which is ordered through the primary care provider and conducted using a low-dose computerized tomography (LDCT) scan of the lungs.

“If the findings on the LDCT are concerning for lung cancer, that patient will be directed to a lung nodule clinic at Northwestern Medicine, where a surgeon and a pulmonologist will review the scan,” says Bharat. “If they concur that the finding is concerning, within a week, the patient will be offered the A-PLUS procedure in the operating room by an interventional pulmonologist and the thoracic surgeon.”
Once in the operating room, Northwestern Medicine patients are met with the newest technology. The first step is a robot-assisted bronchoscopy with live image-guidance, which allows the team to create a GPS-based roadmap of the lung that guides them straight to the tumor.
“We take the CT provided by the radiologist, put it into a robot, and then follow a computer-generated target,” explains Sean Smith, MD, an interventional pulmonologist at Northwestern Memorial Hospital and assistant professor of Medicine in the Division of Pulmonary and Critical Care, as well of Surgery in the Division of Thoracic Surgery.
“What’s special about the robotic scope is that it lets us do biopsies accurately in a minimally invasive way, compared to percutaneous biopsies, which have been the traditional approach, and with which there is a 15 to 20 percent risk of lung injury,” he says. “When we put a needle in through the windpipe, that risk goes down to less than 3 percent.”
While the patient is asleep, the interventional pulmonologist, using the robotic scope, enters through the windpipe and weaves all the way through the dense forest of the lungs into the tiny airways at the edges where early cancers often develop. Once at the target, the interventional pulmonologist removes a small amount of tissue and the sample is then immediately sent to an onsite lab for evaluation. If it is benign, the patient is discharged. If the pathologist determines that the nodule is cancerous, using the same roadmap, the pulmonologist injects an inert dye into the nodule, leaving a dye mark for the surgery. Then, the patient, still asleep, has a second procedure to remove that nodule.
“That’s where A-PLUS really comes in as a true innovation,” Bharat says. “In addition to diagnosing the patient, we are able to treat the cancer using our second robot.”
This second robot has multiple arms, including a camera and other instruments, and allows surgeons to enter the chest cavity through tiny incisions using its 8-millimeter fingers.
“This means that — without cutting through any bone or muscle — we can see the whole lung, identify where the dye marking is, and remove just that tiny segment that is cancerous,” Bharat says.
What’s most remarkable is that the surgeons perform the surgery sitting at a console in the corner of the operating room. “We are performing hand motions while looking at the robot-generated three-dimensional view of the lung with the cancer in it, and the robot is simulating everything we are doing,” Bharat says.
Numerous advantages
The convenience and efficiency of the A-PLUS program are only part of the story.
“The second part of this — which is really key — is that with the dye marking, we don’t have to take a major portion of the lung out,” says Bharat.
Both lungs have parts, called lobes. The right lung has three; the left has two. The traditional approach to lung cancer surgery was to take out the whole lobe, according to Bharat. He uses the analogy of breast cancer, which was at one time treated by removing an entire breast.
“True, if you take the whole lobe out, you will be able to get the tumor out, but the problem is, you can reduce the lung capacity by 25 percent or more,” he says. “Now, we can go into that very specific territory and just remove the one little segment and spare the entire lobe.”
Today’s patients want to be active, he says. They want to be healthy. “And if you take half the lung out, their lung capacity goes down quite a bit, dramatically worsening their quality of life, and they have to stay in the hospital, and then it delays the chemo,” he says.
Another factor, according to Bharat, is that 12 to 15 percent of patients can get a second cancer down the road.
“By taking out only these specific components or segments instead of the lobe leading to lung conservation, we’ve preserved the treatment options in case patients have subsequent tumors,” he says.
Saving as many lives as possible
The new A-PLUS program has come at just the right time. In March, the United States Preventive Services Task Force (USPSTF) updated its lung cancer screening guidelines, making more people than ever eligible. The newly upgraded guidelines reduce the lower limit of the screening age from 55 to 50 years and the minimum smoking history from 30 to 20 pack-years (or one pack on average every day for 20 years). By some estimates, 14.5 million Americans will become candidates for screening — an increase of 6.5 million people, including more high-risk women, and Black and Hispanic smokers, who were previously underrepresented in screened populations.
“With increased screenings, we anticipate that more scans will detect smaller, more peripheral, and earlier stage lung cancers, and the onus will be on our team to facilitate the evaluation and diagnosis of these nodules and potential cancers,” says Smith, adding that as the largest health system in the region with a fully integrated lung cancer diagnosis and surgery program, Northwestern Medicine will be well positioned to help people across Chicagoland and beyond.
“Our goal is that no matter where the patient starts in the system, their evaluation for possible lung cancer — and potentially curative treatment the same day — will be seamless.”
AN ONGOING COMMITMENT TO EARLY DETECTION

Northwestern Medicine has played a key role in life-saving lung cancer screening protocols from day one.
“Historically, we didn’t screen for lung cancer because chest X-rays were shown to be not helpful, but in the early 2000s, Northwestern was a key player in an NIH-sponsored study that looked at LDCT scans as a screening tool,” says Budinger.
In fact, Feinberg’s trial site, headed by Eric Hart, MD, associate professor of Radiology in the Division of Cardiovascular and Thoracic Imaging, was the only one in the Chicagoland area to participate in the National Lung Screening Trial, which lasted from 2002 to 2010 and remains the largest, randomized study ever to demonstrate that screening for lung cancer reduces lung cancer deaths. In 2013, based on study results, the USPSTF began recommending screening, which reduced overall lung cancer mortality of all comers by 20 to 33 percent in high-risk populations, according to The Lancet Respiratory Medicine.
Today, Northwestern Medicine is pushing still further to detect and treat lung cancer early through clinical innovation, according to Bharat. “Simultaneously, we are using state-of-the-art research tools such as molecular and genetic sequencing to engineer patient-specific surgical treatments rather than pursue a generic cookie-cutter approach,” he says.
“Our research goal is to identify molecular and genetic markers in the area of the lung that has an abnormal nodule,” adds Smith. “Traditional biopsies rely on looking at a piece of the nodule under a microscope. Our hypothesis is that we can identify molecular and genetic markers in the nearby tissue that may give clues to the diagnosis, even if the tissue under the microscope is inconclusive.”