The Clinic of the Future
Northwestern Medicine is launching a new digital platform to ensure better care and more face time with patients.
by Martha O’Connell

It may sound like science fiction, but a new “Clinic of the Future” is a about to become a reality — coming soon to Northwestern Medicine Palos Hospital.
Opening in early 2023 at the Palos branch of the Bluhm Cardiovascular Institute, this unique, patient-focused platform will allow providers to spend less time processing medical information and more time addressing the needs of their patients. Powered by unobtrusive digital technology, the clinic will automate the processes of retrieving and storing patient data.
As it stands now, providers spend massive amounts of time inputting information into the electronic health record (EHR) — chronicling medical histories, events between appointments, medications and responses to therapies, images, diagnoses, test results, treatment plans, and more.
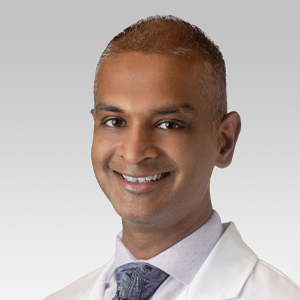
Taking that burden off physicians would be monumental, according to Kannan Mutharasan, ’03 MD, associate professor of Medicine in the Division of Cardiology, and physician champion of this transformative initiative.
“Physicians and providers typically spend 80 percent of the patient visit gathering data and 20 percent of the visit talking about what they are going to do about it. Now, we hope to flip those ratios,” he says.

In this simulation, a patient at the Clinic of the Future is joined remotely by a family member.
A general cardiologist for 20 years, Mutharasan became excited about the potential for change as cloud-based computing skyrocketed more than a decade ago. And yet, years later, paper and CD records still continue to flood him and his colleagues.
“This is just from today,” he says, holding up a four-inch-thick pile.
He is optimistic, however, that the Clinic of the Future will change the status quo.
“I hope this will improve patients’ feelings of being connected to their health provider,” he says. “A big part of this is going to be getting some of the unnecessary distractions of the clinical environment out of the way so we can increase meaningful interactions with our patients.”

Enhancing the patient-physician interaction
The Clinic of the Future was born out of Northwestern Medicine’s Patients First initiative. Experts in artificial intelligence (AI), communications, and patient care came together and envisioned a better hospital experience.
Danny Sama, MBA, vice president of Information Services and chief digital executive at Northwestern Medicine, was among the key coordinators. He explains that the vision is for technology to be embedded everywhere in the Clinic of the Future, yet the tech will be mostly invisible.
A prime example is the way patient data will be collected. AI “conversational intelligence” combined with ambient microphones in patient rooms could take dictation, pick up key terms, and automatically generate visit summaries and diagnostic code choices, as well as other documentation, and put this data into the electronic record — effectively taking documentation responsibilities away from providers. A smart device would also take patients’ vital signs and record them directly in the EHR.
“I think some physicians will be stunned when they have to enter only a few keystrokes to accomplish everything they want to for an entire appointment,” Sama says.
I think some physicians will be stunned when they have to enter only a few keystrokes to accomplish everything they want to for an entire appointment.
Danny Sama, MBA
All the more time for patient-physician interaction — which, too, will be user-friendly. A large wall monitor will show CT scans, graphs showing data over time, or other relevant information, so physicians can explain conditions, treatment plans, or responses to medications, with their patients benefiting from the visual aids.
Ultimately, the Clinic of the Future is designed to help patients get the most out of their visit, Sama says. Even before they enter the clinic, a Northwestern Medicine mobile app will prompt them to think about what they want to discuss and relay it to providers. The app will also ask if they want a family member or loved one to join the appointment; if they do, the participant can attend virtually.
When patients arrive at the clinic, they will get a notification to check in through their phone, then get updates about when the physician will enter their room. Nonetheless, familiar experiences will remain: Nurses will still be present to comfort and assess patients before physicians enter the room.
Not every digital capability described above will be operational when the clinic opens in early 2023. But several smart options will be available for patients to sample. The experimental two-room space will provide the opportunity to try automated functions that might be most beneficial and introduce other digital functions later as they evolve.
A tech-smart space is also planned later next year at Northwestern Medicine’s downtown campus for patients with heart disorders.
The Bluhm Cardiovascular Institute was eager to embrace the Clinic of the Future because cardiac care involves gathering substantial information on heart and vasculature function multiple times over years and years. Patient wearable technology that tracks vitals such as heart rate and blood pressure is becoming common in this “high-touch, high-tech” specialty, making cardiology well-suited for piloting the new concept. However, patients don’t need wearable technology to participate.
A national leader
Northwestern Medicine has significantly built up its cloud infrastructure since 2021, empowering rapid adoption of automation and allowing ideas such as the Clinic of the Future to come to life.
Made possible by St. George Corporation, the initiative was also bolstered when Northwestern Medicine partnered earlier this year with Microsoft to advance digital technology in healthcare. Together with the enormous potential and flexibility of cloud computing, this partnership helped bring the Clinic of the Future to life, putting Northwestern Medicine in a leading position nationally. Elsewhere around the country where digital is envisioned to mesh with healthcare, many ideas remain in the incubation stage.
Efficiency of the clinic will be evaluated to validate that it is actually delivering on its promise. Evidence such as physicians’ time spent on the EHR and patient feedback from satisfaction surveys will be gathered. The goal is an 80/20 ratio of patient time to processing time, but “even a 50-50 split would be huge,” according to Sama.
“Patients don’t come here for our electronic health record,” he says. “They come here for our providers.”