Home / Alumni News / A Career in Neurology
A Career in Neurology
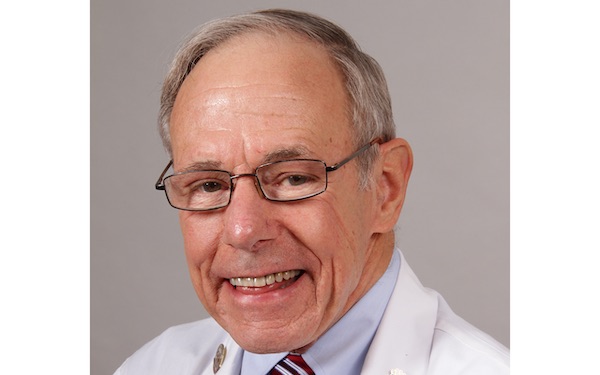
An interview with Sandra Olson, ’63 MD, ’69 GME
illustration by Joel Kimmel

When Sandra Olson ’63 MD, ’69 GME, started at Northwestern’s medical school in 1959, there were four women in her class of 140. This was not unusual; only 5 percent of medical students in the U.S. were women at the time. She went on to achieve many firsts for a woman in medicine — the first to be president of a list of organizations (including the Chicago Medical Society, Chicago Neurological Society, and the Illinois State Medical Society) and the first woman chief of staff at Northwestern Memorial Hospital. But Olson never liked focusing too much on the “first woman” aspect.
It was never my ambition to be president of X, Y, or Z. I took opportunities when they came along.
“I was in the right place at the right time,” says Olson, who is professor emeritus in the Ken and Ruth Davee Department of Neurology. “It was never my ambition to be president of X, Y, or Z. I took opportunities when they came along. It turned out I enjoyed the leadership positions, and I had a proclivity for that aspect of medicine.”
Recently, Olson looked back on her long career and answered some questions.
When did you know that you wanted to be a neurologist?
My interest was piqued during a first-year course in neuroanatomy. We had a session when the professor brought in a patient with Friedreich’s ataxia, a genetic neurodegenerative disorder, and I found it extremely intriguing.
Is there a common attribute that you find among neurologists?
We need to be patient. This is because you don’t see immediate changes in people. For example, a surgeon goes in and fixes a heart and that person is better almost right away. That doesn’t happen a lot in our field. It can take a long time to see a real change in a person’s disease.
What do you love most about the field?
You get to help people, even though you can’t necessarily “cure” the disease. You help them deal with it and work with them to sustain and even improve their quality of life with all the measures at your disposal.
What are some patient stories that have stayed with you all these years?
There are many, but some of them are rather depressing. I remember the 27-year-old, when you had to turn the respirator off. I remember the young woman who had a brain tumor and I was outside the angiogram room with her husband and two children, and I knew what the answer was, and it was bad. Those occasions tear you up. But, there is one happy story that I’ve never forgotten. And that’s a lady who had a pretty mild multiple sclerosis (MS) that came on after she had a baby, which happens. I had seen her early on in my career and I followed her for many years and, fortunately, she was stable all that time. Finally, I said to her one day, “You know, you’re so stable, I don’t think you really have to come back on a regular basis,” and she said, “No, I want to continue to come back and see you and be told that nothing has changed.” That was fine with me. But I still remember the joy in telling her, “You don’t have to come back.”
What are some notable advancements in your field that you witnessed over the course of your career?
There are so many new medications and treatments in the armamentarium now. When I first came out of medical school, we treated MS with steroids. There was a protocol with steroids for 10 days and then a taper. Now you have all these immunotherapies — there are more than a dozen immune-modulating therapies that slow disease progression. Same with migraines — there used be little to offer the many women who came to see me who were debilitated by the headaches. Then, Imitrex changed everything, and now there are so many other options, too.
What do you say to people interested in pursuing a career in neurology?
One in six people will either have a neurological problem or have a close relative with a neurological problem — so there is a need for what we do. But you have to really be patient, like neurology, and be willing to put in the time. Because there are few dramatic fixes in our field.