Home / Alumni News / Opening Doors to Healthier Communities
Opening Doors to Healthier Communities
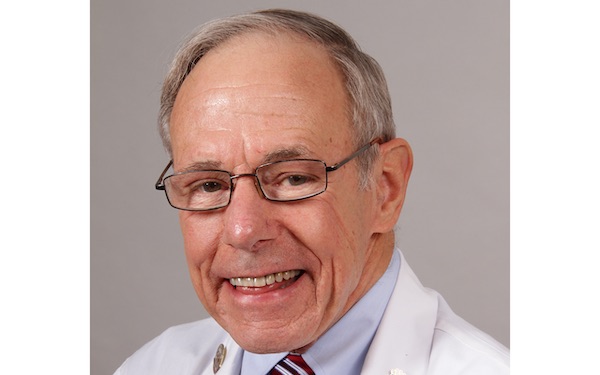
Scott Hamstra, ’85 MD, found the path to caring for marginalized and vulnerable communities while at Feinberg.
By Christina Frank

Scott Hamstra, ’85 MD, credits his time at Northwestern University Feinberg School of Medicine for expanding his horizons and ultimately sparking his interest in improving the health of underserved and vulnerable populations.
“I grew up as a very middle-class, white American male,” says Hamstra. “Northwestern provided a jolt, a remarkable melting pot for exposure and ideas and diversity. We had people from all over the world, and the med students, despite their youth, brought experience that was much wider and deeper than my own.”
Inspired by a Feinberg classmate who grew up in Pakistan, Hamstra traveled to Pakistan with a fellow student for the summer to work in a mission hospital. “It was mind-blowing and eye-opening to experience a very different culture, extreme poverty, and see pathology that is rarely encountered in the United States. This profound experience opened a door to professional possibilities.”
Hamstra’s faculty advisor at Northwestern, the late pediatrician Wayne Borges, MD, encouraged him to pursue pediatrics. Hamstra would go on to do his residency and a fellowship in pediatric infectious disease at Oakland Children’s Hospital in Oakland, California.
“I love the energy and the inherent magic that’s in children to heal,” says Hamstra. “They’re incredibly resilient characters — their immune systems, their bodies, the energy, just the desire to live is amazing.”
In 1990, Hamstra became a U.S. Public Health Officer with the Indian Health Service (IHS) joining a medical staff of 12 at the Whiteriver Indian Hospital that serves the White Mountain Apache Tribe in rural Arizona. At the time, this community, like many other indigenous communities, was contending with a host of infectious diseases, including measles, Hepatitis A, Hemophilus influenza type B, varicella (chickenpox), pneumococcus, and rotavirus, for which vaccines were still in development.
I love the energy and the inherent magic that’s in children to heal. They’re incredibly resilient characters — their immune systems, their bodies, the energy, just the desire to live is amazing.
As vaccines for these diseases became available, the number of cases diminished rapidly. “I saw the very last two cases of hemophilus influenza type B meningitis (Hib) in the spring of 1990,” Hamstra says, before Hib disease was eliminated by vaccination. “Chickenpox was everywhere, and then we got that vaccine and it just disappeared. We implemented the pneumococcal conjugate (PCV7) vaccine, and then that disease too practically disappeared. Enormous credit goes to the community who trusted us and trusted the vaccines.”
Hamstra says he believes that talking about medicine and immunizations in a way that resonates with a specific patient population is critical for demystifying them. “We compare vaccines to seatbelts, and we don’t call them immunizations, we call them shots because that’s what the people call them,” he says. “You get very practical and ask, ‘Who do you want to protect?’ Of course, you want to protect your kids, you want to protect grandma, you want to protect your whole extended family. What if you could do it? What if you could prevent this? As public health officers, we didn’t focus on just one person, we thought about them in context of their family and community.”
When Hamstra first started working in Arizona, he says he and his team were using notebooks to record immunization data. A computer platform called RPMS (Resource and Patient Management System) had been developed by IHS for managing patient information and healthcare resources in the 1980s, but it was not yet widely used across its healthcare facilities until the 1990s.
Northwestern provided a jolt, a remarkable melting pot for exposure and ideas and diversity.
“In hindsight, it’s inconceivable to recall that population level vaccine data was virtually nonexistent in the 1980s,” says Hamstra. “We just watched this medical system get bigger, better, and more robust. There was something uniquely powerful about caring for pretty much everyone in the community, having a community database, and being able to watch diseases disappear as the rate of vaccinations moved from 0 percent to 25 percent to 50 percent to 75 percent. To be able to be part of this combination of advanced science technology and practical application on the clinical front lines and see firsthand the health transformation of a community was astonishing.” Thus, a door to a career in medical informatics opened.
Hamstra led his clinical sites to earn top-ranking awards from the Centers for Disease Control on multiple occasions, with teen and toddler vaccine rates consistently above 90 percent. While he has continued to work with the IHS and American Indian communities in Arizona since retiring in 2014, a new door opened for Hamstra allowing him to use his expertise to improve both pediatric and adult immunization rates among the broader U.S. public in collaboration with public health experts and the American Pharmacist Association Foundation.
Hamstra says he hopes his journey will encourage other students to step outside of their comfort zones. “It’s truly been an adventure, unpredictable, surprising, challenging, and rewarding,” Hamstra says. “I feel extremely privileged and fortunate to have gotten my start at Northwestern. Hopefully my experience will inspire others to ‘Just Say Yes’ to whatever doors people open, because you never know where that next door is going to lead.”