Home / Alumni News / Back to Basics
Back to Basics
Gwendolyn Sowa, MD, PhD, ‘04 GME, leverages her roots in biochemistry to find causes of lower back pain and improve patient care.
By Bridget Kuehn

As co-principal investigator of the National Institute of Arthritis and Musculoskeletal Diseases’ Back Pain Consortium (BACPAC) Mechanistic Research Center, Gwendolyn Sowa, MD, PhD, ’04 GME, endowed professor and chair in the Department of Physical Medicine and Rehabilitation at the University of Pittsburgh, is trying to tease out the underlying causes of low back pain.
She and her multidisciplinary team of colleagues are hoping to translate their discoveries into more personalized, safer, and more effective approaches for treating the leading cause of disability worldwide. In addition to co-leading the BACPAC site at the University of Pittsburgh, she is the co-director of the Ferguson Laboratory for Orthopaedic and Spine Research at the university, medical director of the University of Pittsburgh Medical Center (UPMC) Total Care-Musculoskeletal Health, and director of the UPMC Rehabilitation Institute. Through their patients, Sowa and her colleagues have learned that each patient’s experience with low back pain is different and may be influenced by factors ranging from physical activity to mental health.
“Low back pain is multifactorial,” she explained. “It’s essentially a syndrome and not a specific disease or diagnosis, and that lends itself well to a precision medicine approach that understands what the person is bringing to the table in terms of their own biology, their biomechanics, or how those have changed, and their own beliefs about what types of treatments are acceptable.”
Personalized Approach
During her doctoral studies in biochemistry at the University of Wisconsin-Madison, Sowa decided she wanted her work to be more directly applicable to humans, so she shifted gears and went to medical school at the University of Wisconsin. Her residency at Feinberg and the Rehabilitation Institute of Chicago, now called the Shirley Ryan AbilityLab, allowed her to combine her passion for research with clinical care.
“When I went to Northwestern, there was a lot of support for clinician investigators and a lot of enthusiasm for those pursuing rigorous research,” she said.
The field of rehabilitative medicine hadn’t yet strongly embraced basic research as a means to improve care, she said. However, the supportive environment at Feinberg and the Rehabilitation Institute of Chicago’s reputation as a “mecca for physical medicine and rehabilitation” made it the perfect place for Sowa to combine her biochemistry and medical training to try to help solve pressing patient care challenges.

For the past two decades, Sowa has continued this work at the University of Pittsburgh School of Medicine. There, she’s used her basic research on mechanical loading to understand the sweet spot where exercise can help improve musculoskeletal conditions without contributing to inflammatory conditions.
“Early on, we realized that to do that successfully, we needed a way to measure what was good and bad mechanical loading in a human,” she said. “This made us interested in looking for molecular biomarkers for musculoskeletal pain, particularly low back pain.”
That search has led her to a more holistic approach to assessing low back pain and selecting the best therapies. Sowa explained that she and her colleagues have broadened their search for “biomarkers” to include biomechanical markers, lifestyle factors, environmental factors, and the patient’s experience with pain. She said that all are crucial to selecting the best therapy for a patient.
“It’s definitely not a one-size-fits-all approach,” she said. “We are trying to find the appropriate treatment for the right patient at the right time.”
Creating the Dream Team
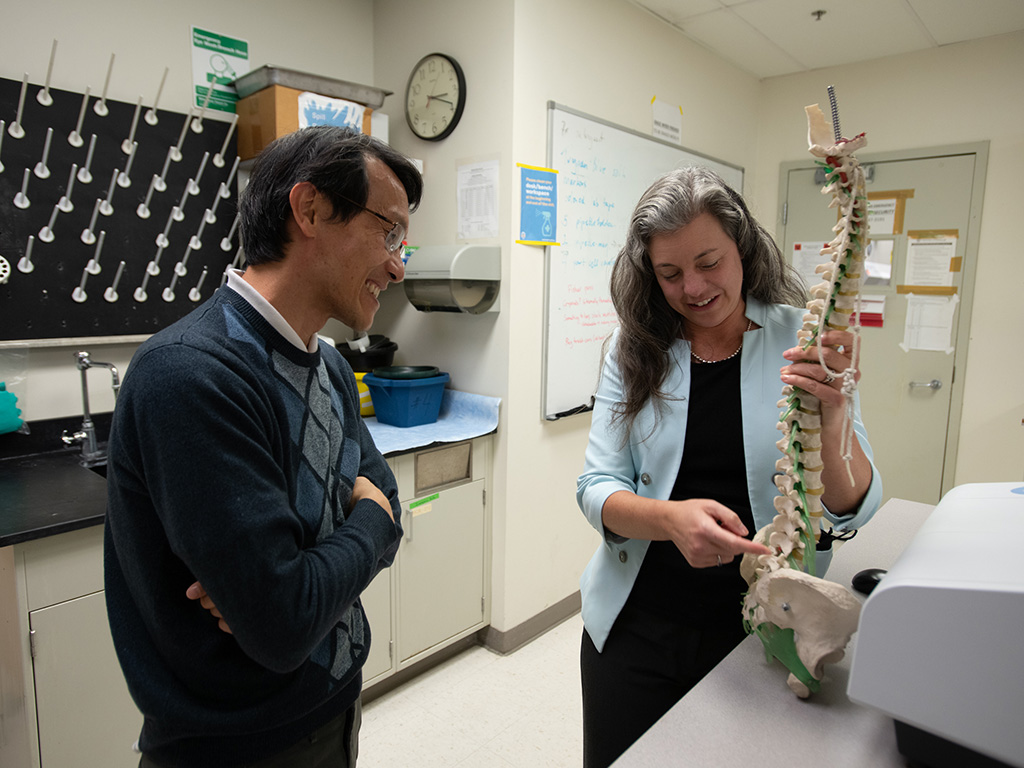
To tackle such a complex problem, Sowa and her BACPAC co-principal investigator Nam Vo, PhD, professor of orthopaedic surgery and deputy vice chair of research in the Department of Orthopaedic Surgery at the University of Pittsburgh, have put together a “dream team” of interdisciplinary specialists and scientists. It includes physiatrists, surgeons, physical therapists, chiropractors, psychologists, molecular biologists, other basic scientists, engineers, biostatisticians, and machine learning experts.
“It’s been the greatest joy of my research career to be able to bring people from very different backgrounds and very different areas of expertise together around this common problem,” Sowa said. “We are working together on a daily and weekly basis to solve this problem in a much more comprehensive way than we’ve ever been able to do before.”
She said her training at Feinberg helped her understand the value of building multidisciplinary teams and taught her how to lead them effectively. The team has already recruited more than 1,000 people with low back pain for the BACPAC study and collected extensive phenotypic information about each patient. Now they are developing models to understand the patients’ molecular, biomechanical, and pain profiles and how they respond to different therapies. According to Sowa, clinicians treating low back pain have historically started with the least invasive approach and progressed from there.
When I went to Northwestern, there was a lot of support for clinician investigators and a lot of enthusiasm for those pursuing rigorous research.
Gwendolyn Sowa, MD, PhD, ‘04 GME
This approach was trial and error and didn’t work very well. Some patients had to undergo unnecessary interventions, and it also led many patients with chronic low back pain to turn to opioid medications, which are not indicated for long-term use in chronic low back pain and also increase the risk of developing an opioid use disorder. The BACPAC study, which is funded in part by the National Institutes of Health’s Helping to End Addiction Long-term (HEAL) Initiative, aims to find safe and effective pain therapies so patients do not find the need to rely on opioids.
“As a medical community, we’ve had a lot of success in starting to decrease unnecessary opioid use,” Sowa said. “We’ve also made some progress treating opioid use disorders. But there remains an important gap — we still need to treat that person’s pain.”
She noted that for most patients with chronic back pain, opioids are not the answer. However, if patients cannot find relief, they may use opioids as a last resort.
“We have to come up with better treatment options so that we do not leave the patients with significant impairment because they can’t participate in their daily activities, their work activities, or their recreational activities,” she said.
The key, she maintains, is matching the therapy to the patient’s needs. However, doing that more effectively will require a lot more actionable data that clinicians can use to guide care. Sowa explained that, currently, clinicians rely on patient reports, imaging, and physical exams.
“If we can equip clinicians with more comprehensive and meaningful data that is actionable and helps them go down a decision tree and select a more effective treatment, we are more likely to have the right outcome the first time,” she said.
As the BACPAC study progresses, Sowa and her colleagues are also deploying multidisciplinary teams in their everyday patient care. Much of their focus is on meeting patients’ goals and selecting treatments that match their needs and interests. For example, Sowa noted some patients want to avoid needles, surgery, or taking medications and would rather focus on lifestyle changes. Team members tap into their diverse perspectives to find the right approach for the individual patient.
Bench to Bedside
Sowa’s bench-to-bedside approach has gained her national recognition as a leader in the field of physical medicine and rehabilitation. She served as president of the Association of Academic Physiatrists (AAP) from 2021 to 2023 and is finishing her term as the organization’s immediate past president. She said she relished the opportunity to give back to an organization that has been a source of support throughout her career and a place where she has made lasting friendships.
“We’ve been able to elevate the field and be a resource for people at all stages of their careers and help them find support,” she said. During her leadership, AAP grew in size and international reach.
She has also earned recognition beyond her field. In 2022, Sowa was inducted into the National Academy of Medicine. She attended her first meeting last year and said being asked to join was one of the proudest moments of her career. “I was kind of a fan girl with a lot of the scientists who were there,” she professed. “It was amazing to meet some of these people.”
Sowa is also a vocal advocate for more basic science training for physicians. It’s something that is essential in order to be a good physician, particularly as clinicians increasingly have more data at their fingertips and must use critical thinking skills to put it to the best use, she noted.
“A good clinician uses the scientific method in their work,” she said. “There is no protocol that fits every patient, it is about collecting data, developing an informed hypothesis, and using testing to validate or refute that hypothesis. When clinicians use this method, they are less likely to miss things.”
It’s an approach she aims to instill in her trainees, whom she encourages to pursue careers as physician-scientists. She noted that having support and mentorship, as she did at Feinberg, is critical because a physician-scientist’s path isn’t always straightforward. But it can be incredibly rewarding.
“Being able to see patients and bring those questions back to your research and then have your research inform what you do clinically is super meaningful,” she said.