Breathing New Life
Northwestern Medicine team provides life-saving cancer treatment to expectant mother.
By Amanda Dee | Photography by Laura Brown, Northwestern Medicine

MaKenna Johnson and her husband, Parker, live on a farm nestled in the middle of Illinois. While MaKenna was pregnant, she continued to wake early to feed the horses and chickens and let the animals roam. In the afternoon, she would bring them back in and top off their food and water. That is, until a persistent dry cough disrupted her routine.
“My body felt like I just ran two miles, when in reality, I had only walked to the barn and back,” MaKenna said. “I’ve had lupus my whole life. I know my body. I knew something was wrong.”
Her local care team was wary of performing scans due to potential radiation exposure for the baby, so they watched and waited, and things got worse. During her third trimester, she coughed so hard she started vomiting.
Then MaKenna began to struggle to breathe. Local physicians found, through imaging, a tumor the size of a grapefruit. The tumor sat on her heart and three lobes of the right lung, obstructing the pulmonary artery. She was in respiratory distress, and the local hospital wasn’t equipped to handle such a case. She would need to be flown to Northwestern Memorial Hospital.
As MaKenna’s family abandoned their original plans for this major life event, specialists across Northwestern Medicine began planning to save MaKenna and her baby.
THE DELIVERY TEAM
On Easter weekend, a team of obstetricians, surgeons, anesthesiologists, pediatricians, and nurses awaited MaKenna in the middle of the night. They had no time to waste. MaKenna had started having contractions, and her blood pressure was rising. Neither she nor the baby was getting enough oxygen. Physicians would need to perform a cesarean birth.
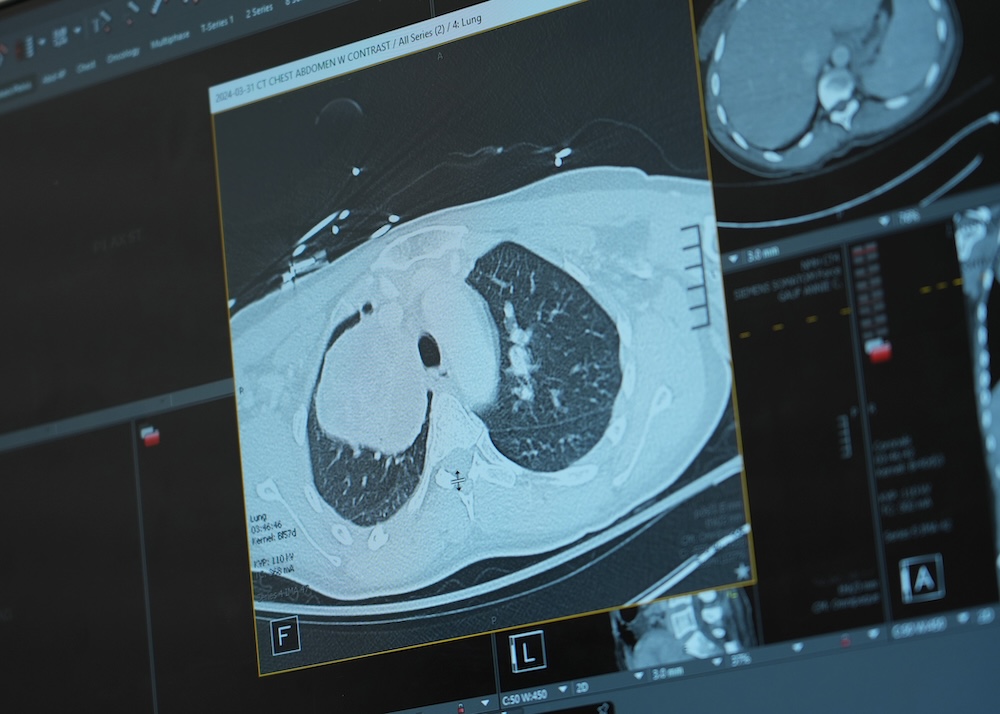
Local physicians found, through imaging, a tumor the size of a grapefruit.
To prepare for surgical birth, the maternal-fetal medicine team worked with the adult and neonatal intensive care unit and vascular surgery teams. Nurses hurried from Prentice Women’s Hospital to support the delivering physician, Lynn Yee, ’08 MD, ’08 MPH, the Thomas J. Watkins Memorial Professor of Obstetrics and Gynecology in the Division of Maternal-Fetal Medicine, in the ICU and Feinberg Pavilion operating rooms.
“From the second we were at Northwestern, it was a completely different world,” observed MaKenna’s husband, Parker. “The professionalism of everyone and how on task they were and the expertise there — it was like something out of a TV show.”
In the early morning of March 31, Yee delivered their son, a healthy baby boy whom they named Colter.
THE CANCER TEAM
Before surgeons and oncologists could treat MaKenna’s tumor, they needed to know more about what they were dealing with. Kalvin Lung, MD, assistant professor of Surgery, led the efforts to identify the tumor type. Using advanced bronchoscopy, Lung diagnosed MaKenna with stage 3 melanoma. Because the tumor extended toward the heart, Lung reached out to his department colleague Christopher Mehta, MD, assistant professor of Surgery in the Division of Cardiac Surgery, who specializes in complex heart reconstruction at the Bluhm Cardiovascular Institute.
“It’s extremely rare to see this type of tumor invading into the major blood vessels of the heart,” Mehta said. “We may see something like this once every few years.”
Lung operates within the Canning Thoracic Institute, which was established to handle complex cases like MaKenna’s.


“We move beyond our own cancer circles,” Lung said. “For example, this melanoma case was presented at the thoracic oncology tumor board first, and then we brought it to the melanoma tumor board because that’s where the expertise was.”
Lung specifically consulted Sunandana Chandra, MD, MS, associate professor of Medicine in the Division of Hematology and Oncology, and a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
“We think at some point, MaKenna had a melanoma on her skin and her own immune system took care of it, but not before a cell or two may have escaped and eventually started growing inside her body,” Chandra explained.
Per Chandra’s recommendation, MaKenna underwent immunotherapy prior to surgery, which reduced the tumor by 30 percent, to 9 centimeters.
Rare cases such as this can benefit tremendously from the insights in clinical trials, especially when time is of the essence. In one nationwide clinical trial with Northwestern Medicine participants, investigators discovered the benefits of pre-surgical immunotherapy on surgical outcomes for advanced melanoma patients. The results of this clinical trial guided Chandra’s recommendation.

“We know that particularly in lung cancer and certainly in melanoma, in the recent five to 10 years, we’ve had so many more developments in medicine — chemotherapies, targeted therapies, immunotherapies — that have really benefited our patients,” Lung said. “If we weren’t ahead in these clinical trials, the last 10 years of patients would not have had the same level of treatment.”
After three rounds of immunotherapy, Lung and Mehta removed MaKenna’s right lung and sections of the main pulmonary artery and lymph nodes.
“MaKenna’s scans currently show no evidence of metastatic melanoma, and the hope is with continued surveillance, we’ll continue to show she has no evidence of disease,” Chandra said. “Medically, this is an amazing story with profound results. This type of outcome for our patients is what we always hope for.”
ALL TEAMS GO
After Colter’s delivery, his parents grieved the unexpected cancer diagnosis and the distance from their son. While Colter stayed in the NICU for a week, they moved between the hospital and a small room nearby, hours from their home. The family’s extended care team tried to support them during this difficult time. Parker expressed gratitude for Yee’s ongoing communication with them.
“Dr. Yee made sure she was always there regardless of where MaKenna was put in the hospital,” Parker said. “She wanted to make sure even if MaKenna wasn’t in the women’s hospital she would have the same care.”
“The family members are as much our patients as anybody,” Yee said.
Yee also stressed that collaboration at Northwestern isn’t limited to the physicians and scientists: “One thing about Northwestern Medicine that makes me feel really proud to work here is our outstanding team members, all of the technicians and nurses and medical assistants who are dedicated to the care of these complex patients.”
Both MaKenna and her husband singled out clinical nurse Mary Schuessler, a lifeline when their son was in the NICU.
“This type of outcome for our patients is what we always hope for.”
Sunandana Chandra, MD, MS
“I knew for a fact that Colter was extremely well taken care of in my absence. Mary kept me informed on every little thing, and she wouldn’t sugarcoat things,” MaKenna said. “She was probably the most important person throughout my entire stay.”
Schuessler understood they felt far from home, Parker said, and she tried to make them feel closer to it.
BACK ON THE FARM
This April, baby Colter celebrated his first birthday. MaKenna finished a year of immunotherapy treatments. While she now gets winded more easily, her routine has almost returned to what it once was — as much as any routine can in Midwestern spring. When the temperature dropped early that month, the family had to open up their kitchen to newly hatched chicks.
Almost nothing about Colter’s birth went as the family had expected, but Parker called Northwestern a “blessing.”
I’m so grateful to have Colter and Parker in my life, and I can’t say enough about the wonderful medical team that saved my life,” MaKenna said. “Because of Northwestern Medicine, I’m here today.”












