by MELISSA ROHMAN | photography by TERESA CRAWFORD
Searching for answers when diagnosis is elusive
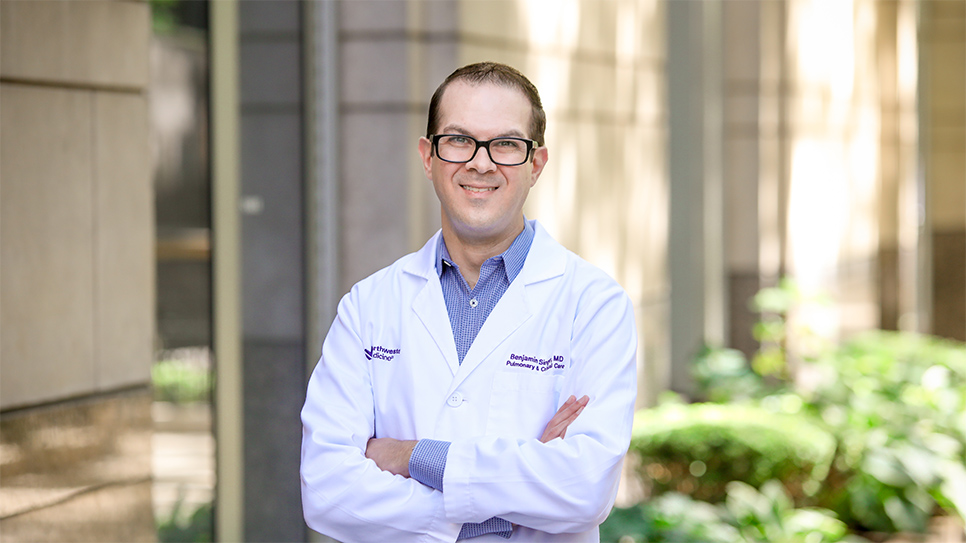
In 2015, Benjamin Singer, ’07 MD, ’10 GME, joined Feinberg as an assistant professor of Medicine in the Division of Pulmonary and Critical Care and of Biochemistry and Molecular Genetics. That same year, under the direction of Douglas Vaughan, MD, chair and the Irving S. Cutter Professor of Medicine, Singer also established the Socrates Project, a first of its kind physician-to-physician consultation service that helps Northwestern Medicine referring physicians diagnose diseases that are challenging to identify.
Using Socratic principles, particularly iterative hypothesis testing, the aim of the project is to improve patient care by providing diagnostic possibilities and recommendations to referring physicians with the overarching goal of reducing or managing diagnostic uncertainty.
“We work at one of the top medical centers on the planet with some of the smartest specialists and subspecialists that you can find, but that doesn’t always mean that patients come away with a confirmed diagnosis,” Singer says. “There are still patients who have unexplained signs and symptoms, so the idea was that we could help fill that unmet need.”
The service team is led by Singer and is composed of Feinberg’s chief medical residents. Residents spend one extra year after their residency volunteering on the team to focus on education and administration, with one of the residents assuming primary responsibility for each new consultation request the service receives. Due to COVID-19, the team has been conducting all service operations virtually.

Probing Diagnostic Unknowns
“The Socrates project has challenged me to think critically and entertain diagnoses that I once would not have. Most importantly, it’s humbled me as a physician, exposed the complexity of the human body, and pushed me to sometimes be okay with diagnostic unknowns,” says Sneha Thatipelli, MD, ’20 GME, chief medical resident in the Department of Internal Medicine, who is on the Socrates team.
The team receives about two consultation requests per week, usually submitted by Northwestern Medicine general internists, but also from specialists of all disciplines. According to Singer, roughly 80 percent of the referrals are for current inpatients at Northwestern Memorial Hospital, and there is no additional charge to patients when physicians use the consultation service.
After obtaining the patient’s case history from the referring physician, a resident conducts thorough reviews of medical literature and electronic health records. The resident will also reach out to experts either at Feinberg or across the country to devise diagnostic possibilities and testing recommendations. In the inpatient setting, the resident performs a new patient history and physical via telemedicine to construct a detailed list of the patient’s health problems.
Singer then reviews and refines the list and diagnostic possibilities with the resident, which are then shared with a larger review team consisting of volunteer general internists, specialists, and the rest of the Socrates team. Finally, the service team will document the patient’s health problems, diagnostic possibilities, and recommendations in the patient’s medical record and discuss the case with the referring physician and their team.
The turnaround time for this process is one week, according to Singer, but can be done faster for more urgent cases.
“In almost all cases, the referring physicians have done an incredible job with the workup and we either validate what they’ve done or recommend other things that might be helpful in this patient’s case,” Singer says.
No Lone Healers
Overall, the service limits its clinical recommendation to diagnosis and avoids commenting on management decisions outside of the use of therapies as diagnostic tests. Oftentimes, however, the team is unable to come up with a concrete diagnosis. This, according to Singer, is because the diagnosis may be identifiable, just not by the Socrates Projects physicians involved in the case or the physicians they consulted (it simply isn’t plausible to ask every physician across the globe to exhaust the possibility of a knowledge deficit, he explains). The other reasons why a concrete diagnosis isn’t possible, he says, are: The diagnosis is a described condition without any available tests, or the diagnosis has not yet been described by medical science — for example, seeing a case of COVID-19 at the end of 2019.
Arushi Singh, MD, ’20 GME, chief medical resident in the Department of Internal Medicine and a member of the Socrates team, has been working to understand a particularly challenging patient case over the past few weeks, involving various subspecialty physicians across centers of care around the country.
“This case has required multiple weeks of investigation, and we have yet to arrive at a final diagnosis. The process has been trying, but I have derived patience and support from my colleagues and Dr. Singer. It is a work in progress, and I am hopeful that more information will come to light through the test of time,” says Singh.
For Singh, the Socrates Project has reoriented her perspective on patient care and has provided her with the opportunity to gain news skills she hopes to apply throughout her medical journey.
“It’s a reminder of the importance of having physicians step back and look at the complexities of a patient presentation across subspecialties in their entirety. In addition, it has pushed me to develop and organize my diagnostic reasoning skills in collaboration with trusted friends and mentors,” says Singh.
Continued review and cataloging of other similar patient cases and data for educational purposes is paramount. The service has an established follow-up system for cases, which involves team members reviewing patient charts and reporting them during the team’s weekly meetings, as well as making regular phone calls to patients and providers for cases that haven’t been followed up on for a while due to missed appointments and documentation or unreturned phone calls from providers.
“We never just throw up our hands and say we have no idea,” says Singer. “We’ll always have an idea, we’ll always have a list, but whether we can prove it definitively or not is a different question.”
As for the future of the Socrates Project, Singer says he hopes to expand the team and continue to see the program emphasize how medicine is truly a “team sport.”
“The idea of the lone healer going out there and helping a patient — that’s not how we should practice best as physicians,” he says. “We should talk to each other, and that’s why it’s great when physicians reach out to us so we can have those conversations and try to ultimately get an idea out there that will help the patient.”
It’s a reminder of the importance of having physicians step back and look at the complexities of a patient presentation across subspecialties in their entirety.
Arushi Singh, MD