Clearing Pathways
The Simpson Querrey Lung Institute for Translational Science (SQLIFTS) ushers in a new era of lung research, education, and patient care.
by Gina Bazer
photography by Gr8y Productions
In the last few years, advancements in the study and treatment of lung disease at Northwestern Medicine have been extraordinary. With the onset of the pandemic, Feinberg scientists made discoveries at breakneck speed — from the first examination of cells in the lungs of patients with COVID-19 pneumonia, published in Nature, to the first-ever lung transplant performed on a patient with COVID-19, conducted at Northwestern Memorial Hospital and documented in Science Translational Medicine. The team’s clinical findings with more than 40 of these patients has also been published in JAMA.
In addition to COVID-19, the Division of Pulmonary and Critical Care has been steadily chipping away at the many other obstacles that plague lung health and treatment. One such pursuit, described in Proceedings of the National Academy of the Sciences, identified lung epithelial cells with stem-cell-like qualities that could provide promising therapeutic pathways for pulmonary fibrosis. In another study, published in the Journal of Clinical Investigation, Feinberg investigators uncovered a protein that acts as a “molecular brake” that could reduce lung transplant failure, which, lamentably, happens in almost half of recipients.
Meanwhile, new studies are about to launch. Last fall, a group of Northwestern Medicine investigators received a $14 million grant from the National Institutes of Health’s National Heart, Lung, and Blood Institute to study viral pneumonia.
In short, the momentum in the division is remarkable, and the progress exemplifies the transformative power of translational science — which is made possible when patient care is seamlessly integrated with research, according to Scott Budinger, MD, chief of Pulmonary and Critical Care in the Department of Medicine.
“Every patient coming into our medical center should have an opportunity to participate in research that will advance knowledge about the disease from which they suffer,” says Budinger, who is also the Ernest S. Bazley Professor of Airway Diseases.
To fully realize the immense potential of this bedside-to-bench-to-bedside approach, Feinberg has launched the new Simpson Querrey Lung Institute for Translational Science (SQLIFTS), made possible thanks to a generous gift from Northwestern trustee Kimberly Querrey and the Louis Simpson Trust.
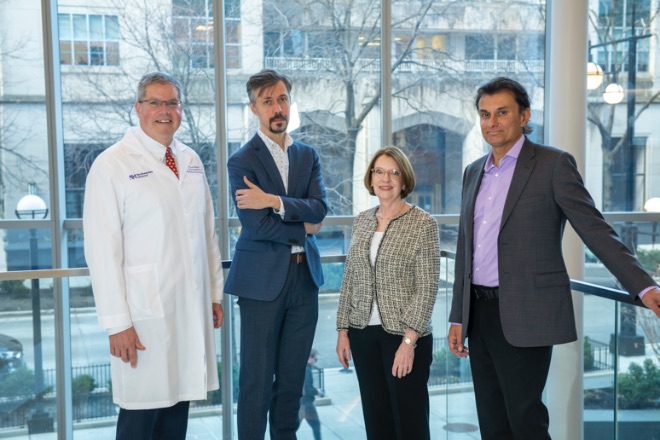
Budinger will serve as executive director of the institute, which is made up of four programs: the SQLIFTS Translational Innovation Program, the SQLIFTS Technology Program, the SQLIFTS Discovery Program, and the SQLIFTS Health Education Program.
Improving quality of life
The launch of the institute happens at a critical time, as the data about lung disease is alarming. Even before the pandemic, pneumonia was the most common cause of death from an infectious disease worldwide. Briefly eclipsed by COVID-19, chronic obstructive pulmonary disease (COPD) will likely again become the third leading cause of death in the United States. And deaths from lung cancer outnumber all other forms of cancer combined. Just as concerning are the many trickle-down effects of lung disease on other organs.
“The impact of lung disease on quality of life is profound,” Budinger says. “It accelerates dementia, skeletal muscle dysfunction, renal failure, and cardiovascular disease. But what’s so powerful about the SQLIFTS model is that much of the work we are doing here is tissue-agnostic. The discoveries we make here, the technologies we create, will be applicable to a range of diseases.”
The discoveries we make here, the technologies, we create, will be applicable to a range of diseases.
SCOTT BUDINGER, MD

Fostering translational science
A partnership between SQLIFTS and the Canning Thoracic Institute (CTI) at Northwestern Memorial Hospital, the SQLIFTS Translational Innovation Program will offer patients across Northwestern Medicine’s 11-hospital health system the opportunity to participate in research. The program will be directed by Ankit Bharat, MD, chief of Thoracic Surgery and executive director of CTI.
During the height of the pandemic, Bharat was able to perform the first lung transplant for a patient with COVID-19 in the U.S. due to key findings about the mechanisms of the disease that were discovered in Feinberg laboratories. Since then, Northwestern Medicine has performed 45 lung transplants for patients with COVID-19. The division has also developed the innovative Ambulatory Precision LUng Sparing (A-PLUS) program, which not only allows for the diagnosis and surgical treatment of lung cancer in a one-day outpatient procedure, but also offers another opportunity for sample collection.
The Canning Institute is a hub for clinical innovation that finds its roots in laboratory and clinical science, creating the perfect synergy with SQLIFTS.
Ankit Bharat, MD
“The Canning Institute is a hub for clinical innovation that finds its roots in laboratory and clinical science, creating the perfect synergy with SQLIFTS,” says Bharat. “This partnership will provide investigators who study diseases of the chest easy access to tissue that will allow them to develop novel therapeutics, run trials to validate biomarkers, and administer rapid diagnostic tests for personalized medicine.”
Leveraging emerging technologies
Cutting-edge multimodal technologies are leading to a better understanding of all types of disease at the molecular level, and the goal of the SQLIFTS Technology Program is to harness these new approaches for the study of lung disease. Furthermore, technologies validated in the lung can be shared with investigators across Northwestern to be applied to other areas of study, according to program director Alexander Misharin, MD, PhD, associate professor of Medicine in the Division of Pulmonary and Critical Care.
Misharin himself is a trailblazer in the application of genomic technologies to the study of lung disease. His laboratory published the first single cell RNA-sequencing analysis of the normal and fibrotic human lung, and he also led the Chan Zuckerberg Human Lung Cell Atlas project, which has integrated data across laboratories worldwide to create a molecular atlas of the more than 40 distinct cell populations that comprise the lung.
But the advancements made through this program will reach beyond the laboratory. “High-resolution pathology must be interpreted in the context of the patient’s clinical course,” says Misharin. “So, a major focus of the center is to develop tools to extract and analyze data from the electronic health record using machine learning approaches, allowing the detailed but sparse molecular pathology obtained during clinical care to be interpreted alongside clinical imaging data, clinical visits, and even wearables to ultimately create a personalized care plan for patients.”
Catalyzing therapeutic development
With a solid infrastructure in place for extracting clinical and genomic data, the SQLIFTS Discovery Program, under the leadership of Navdeep Chandel, PhD, will work with investigators to develop causal models and test innovative hypotheses to identify culprits in the development of lung disease.
Chandel, who is the David W. Cugell, MD, Professor of Medicine in the Division of Pulmonary and Critical Care and of Biochemistry and Molecular Genetics, has demonstrated the critical role mitochondria play in both homeostasis and diseases, including cancer, in effect changing the scientific view of mitochondria from “powerhouses” of energy metabolism to “signaling organelles.” His laboratory uses causal genetic interventions to target key pathways in metabolism to dissect mitochondria’s role in cellular and animal models of disease. The Chandel laboratory has already generated murine, organoid, and cellular models of lung disease.
“The tools and conceptual frameworks we are generating will accelerate the pace of therapeutic development,” Chandel says.
The program will partner with Northwestern’s Innovation and New Ventures Office (INVO) and industry to bring validated targets for therapy to the clinic.
Training the next generation
Led by Karen Ridge, PhD, the SQLIFTS Health Education Program will ensure that the crucial study of the respiratory system continues to flourish for decades to come at Northwestern. Ridge, who is the Ernest S. Bazley Professor of Pulmonary Sciences and a professor of Cell and Developmental Biology, has already made critical discoveries about the mechanisms by which the lung repairs after injury, particularly in viral pneumonia.
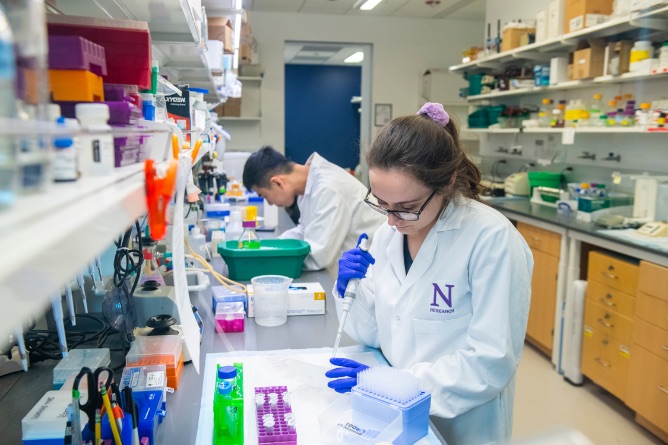
Ridge is relentlessly focused on education, serving as the principal investigator of the NIH T32 Training Program in Lung Sciences, which supports the development of predoctoral and postdoctoral candidates. Ridge also directs the Kimberly Querrey Summer Research Program, which offers high school and college students the opportunity to participate in research, and the Cugell Fellowship for foreign trainees, supported by a gift from David Cugell, MD, the first Chief of Pulmonary Medicine at Northwestern. Additionally, under Ridge’s guidance, SQLIFTS will support the new Simpson Querrey Fellowship in Data Science.
“SQLIFTS is committed to growing a scientific workforce that reflects the rich diversity of the patients we serve,” Ridge says. “This starts as early as high school and continues on through residency and beyond. Our structured programs will put scientists and physician scientists from all backgrounds on paths to successful careers in lung health.”