Trusting Your Gut
Feinberg faculty study how the gut’s microbiome affects a wide range of conditions.
By Cheryl SooHoo
Having “good” intestines may be the key to good health. Maintaining a gastrointestinal (GI) tract full of friendly bacteria remains a hot topic for preventing and treating disease. It is now known that the GI tract and the central nervous system communicate via a microbiota-gut-brain axis, leading some to describe the gut microbiome as a “second brain.” Mounting evidence points toward the critical role the gut microbiome plays in myriad disorders ranging from intestinal to neurological and vascular conditions.
In this still-emerging area, Northwestern investigators are exploring how to best leverage the gut microbiome to improve health outcomes. Their novel work ranges from developing innovative diagnostics and treatments to understanding how gut microbiota impact the molecular underpinnings of a range of conditions.
DIAGNOSTIC PROBIOTIC
Some three million Americans suffer from inflammatory bowel disease, according to the Centers for Disease Control and Prevention. Simply known as IBD, this GI disorder causes persistent diarrhea, abdominal pain, weight loss, and permanent damage to the digestive system.
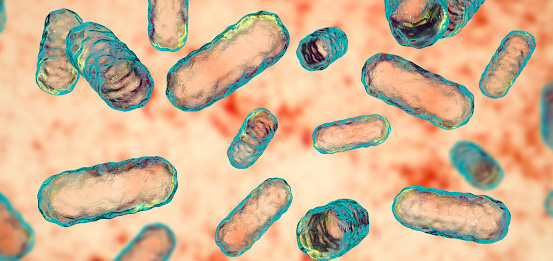
Today, monitoring IBD requires invasive endoscopy and colonoscopy procedures, and predicting flare-ups is a guessing game. Harnessing recent advancements in synthetic biology approaches, Northwestern Medicine scientists have engineered a probiotic capable of noninvasively detecting inflammatory bowel disease. In a study published in the Proceedings of the National Academy of Sciences (PNAS), the investigators manipulated the beneficial bacterium E. coli Nissle by adding a protein capable of detecting a known biomarker for IBD.
“The human body contains millions of microbiota, bacteria that are part of healthy, normal human biology,” says senior author of the study Arthur Prindle, PhD, assistant professor of Biochemistry and Molecular Genetics and of Microbiology-Immunology. “We wondered whether those very bacteria could be repurposed to actually sense biomarkers of disease as a way of monitoring and tracking inflammatory bowel disease in humans.”
The Prindle lab’s discovery of a novel transcriptional response to the IBD biomarker calprotectin paved the way for developing an innovative diagnostic. The engineered probiotic works by sensing calprotectin and changing its gene expression and response. Piggybacking on a natural response, the synthetic sensor produces a measurable output that can be used to detect the presence of disease, according to Prindle.
The current gold standard of IBD monitoring involves expensive, time-consuming, and invasive means. What we hope to do is use probiotics as a less invasive and less costly readout of disease.
Arthur Prindle, PhD
The potential for a more patient-friendly diagnostic tool for IBD offers much promise for simply detecting and monitoring a variety of human diseases. “The current gold standard of IBD monitoring involves expensive, time-consuming, and invasive means,” says Prindle. “What we hope to do is use probiotics as a less invasive and less costly readout of disease.”
FOOD FOR THOUGHT
While the gut may seem far from the brain, it has become increasingly clear that the two communicate via the microbiota-gut-brain axis. Running from the brain and through the entire GI tract, the vagus nerve serves as an information highway by relaying chatter between microbiota metabolites and the brain. In animal models, studies have shown that injury to the brain can deplete good bacteria living in the GI tract. These changes can result in gut inflammation, which has been hypothesized to contribute to the harmful neural inflammation often caused by traumatic brain injury (TBI).
A trauma surgeon with a background in immunology, Steve Schwulst, MD, associate professor of Surgery, and his team, which includes gut specialist and postdoctoral fellow Booker Davis IV, PhD, have been investigating how the gut microbiome and brain’s immune system can influence healing after brain trauma in mice. When the brain is injured, the brain’s immune cells (called microglia) become activated. While normally protective in fighting disease, this activation can trigger chronic uncontrolled low-level neuroinflammation that has also been implicated in neurodegenerative diseases like Alzheimer’s, Parkinson’s, and related dementias.
Schwulst wondered if this neuroinflammation was being fueled by changes in the gut microbiome. Could restoring a pre-injury gut microbiome make a difference? Performing fecal microbiota transplants, the Schwulst team transferred stool from healthy young mice into brain-injured mice. After undergoing doses of healthy gut bacteria, the TBI mice showed marked improvements in their learning and memory capabilities. The therapy appeared to quickly provide significant neural protection.
Whether it’s a stool transplant or replacing certain metabolites, what we are doing is making changes to the overall gut microbial community structure. This treatment paradigm could hold much promise for treating myriad brain diseases in the future.
Steve Schwulst, MD
“It was truly striking to see the results,” Schwulst says. “Imagine a car accident victim comes into the hospital with a TBI and you could restore their gut microbial community structure to its pre-injury state with a simple stool transplant. The clinical implications are profound.”
In other studies, the investigators have gathered data that shows TBI decreases a type of gut bacteria that ferments dietary fiber into anti-inflammatory short-chain fatty acids. When the Schwulst lab added the beneficial fatty acids into drinking water provided to TBI-induced mice, the investigators noted enhanced protection of neurocognitive abilities in the animal model. These findings provide interesting food for thought for the potential of using supplements to improve brain injury as well as other neurodegenerative conditions, according to Schwulst.
“Whether it’s a stool transplant or replacing certain metabolites, what we are doing is making changes to the overall gut microbial community structure,” he says. “This treatment paradigm could hold much promise for treating myriad brain diseases in the future.”
PROTECTIVE SUPPLEMENTATION
Clogging of the blood vessels, or atherosclerosis, often requires vascular “plumbing” to avoid heart attack, stroke, amputation, or death. Patients routinely undergo procedures such as balloon angioplasty, stenting, or bypass surgery to remove or get around blockages or “narrowings” impeding blood flow. Yet for some 30 to 50 percent of patients, these interventions can cause an inflammatory response that leads to scarring or neointimal hyperplasia and gradual re-narrowing (restenosis) of the blood vessels.
The gut microbiome’s influence on inflammation and wound healing has long driven the work of Karen Ho, MD, the John Marquardt Clinical Research Professor of Vascular Surgery. As a vascular surgeon, she has a keen interest in improving surgical outcomes. “When patients develop restenosis, they may need more surgery or a different type of operation, for example, to preserve a limb,” Ho maintains.
Investigating how gut microbes may affect atherosclerosis and arterial remodeling after arterial “injury,” the Ho laboratory has steadily connected the dots.
By boosting the microbes that produce butyrate or trying other microbe-targeted strategies, perhaps we can reduce the risk or develop novel drugs to prevent restenosis.
Karen Ho, MD
First, the team conducted metabolomics studies analyzing blood samples from patients with advanced peripheral artery disease compared to those without. The investigators discovered a connection between certain metabolites and the severity of disease. Then in 2018, Ho and her colleagues were one of the first to demonstrate the effect of gut bacteria on peripheral blood vessels in a mouse model and establish a direct link between microbiota and the development of restenosis after vascular procedures. Using germ-free mice born in completely sterile conditions and lacking microbiota, the investigators compared the animals’ arterial injury response with a group of conventional mice. They found that the germ-free mice had less scarring as well as a decreased inflammatory response, lending support to the influence of microbiota on blood vessel repair. After fecal transplantation using stool from conventional mice, the scarring response after surgery was again observed.
In recent work, the team has focused on the role of supplementing butyrate — a short-chain fatty acid within the same group of metabolites being studied by the Schwulst lab — to prevent scarring and restenosis after arterial injury. “Our thought is if we can modulate inflammation, maybe we can affect how a patient responds to vascular surgery,” Ho says. Using mice that lacked a receptor for butyrate, the investigators found that these animals developed more restenosis than their healthy counterparts in response to arterial injury. When the mice received butyrate, they developed less scarring and restenosis of their blood vessels.
Supported by a National Institutes of Health RO1 grant, the Ho team is now looking at the mechanism of how butyrate works within cells. “By boosting the microbes that produce butyrate or trying other microbe-targeted strategies, perhaps we can reduce the risk or develop novel drugs to prevent restenosis,” she says.
UPENDING ASSUMPTIONS
Given their location, many gut bacteria aid in digestion and metabolism. The gut microbiome’s possible influence on obesity has generated a great deal of interest as a promising therapeutic target to fight a growing public health concern. While myriad studies in adults and models of mature animals have suggested a causal relationship, very little research has focused on the impact of GI bacteria on obese children and teens. Enter the Pediatric Obesity Microbiome & Metabolism Study (POMMS), part of a National Institute of Diabetes and Digestive and Kidney Diseases study to define the role microbiota may play in weight gain and loss in youth.
“Our aim is to close the gap in the understanding of the microbiome’s effect on obesity and metabolic syndrome in adolescents,” says Patrick Seed, MD, PhD, president and chief research officer of the Stanley Manne Children’s Research Institute at Ann & Robert H. Lurie Children’s Hospital of Chicago. A professor of Pediatrics in the Division of Infectious Diseases, of Microbiology-Immunology and the Children’s Research Fund Professor of Basic Science, Seed serves as the co-principal investigator of the multi-center (Northwestern, Duke University, and the University of North Carolina at Chapel Hill) POMMS.
Launched in 2016, the longitudinal study followed 350 patients, ages 10 to 18: one group undergoing treatment for obesity and another group of healthy youth of similar ages. In an analysis of microbiome and metabolomic data, Seed and the POMMS investigators have upended the growing literature on the gut microbiome’s impact on individuals across their entire life span.
Our aim is to close the gap in the understanding of the microbiome’s effect on obesity and metabolic syndrome in adolescents.
Patrick Seed, MD, PhD
“Even though the kids had severe obesity and associated metabolic changes, we found their microbiomes did not differ much from that of healthy controls,” Seed contends. “Our data defies the idea that major shifts in the microbiome are an essential ingredient of obesity and metabolic syndrome for every life stage. Once again, children are not just small adults. Or in adults, maybe we don’t have the whole story.”
Seed hypothesizes adolescents may have a certain plasticity and resiliency to metabolic dysregulation. In other preclinical studies, the Seed lab is now trying to understand what adaptations to specific organisms may give youth protective factors against metabolic drivers of obesity.
ADVANCES TO COME
At Northwestern, gut microbiome research continues to gain traction. In October, Feinberg welcomed Yingzi Cong, PhD, a leading microbiome scientist who studies the immune regulation of host-microbiome interaction in the development of inflammatory bowel diseases as well as the role of gut microbiota in producing metabolites that regulate various immune responses and disease conditions. His group was among the first to demonstrate the crucial protective role of T-cells specific for a gut microbiota antigen in the regulation of intestinal inflammation. He was most recently director of microbiome research at the University of Texas Medical Branch in Galveston. Cong’s work has been published in Nature Communications, Gastroenterology, Journal of Experimental Medicine, and PNAS. A professor of Medicine in the Division of Gastroenterology and Hepatology, he will be a key leader of new microbiome-based research in the Center for Human Immunobiology (CHI).
“The microbiome field is still very young,” says Stephanie Eisenbarth, MD, PhD, chief of the Division of Allergy and Immunology in the Department of Medicine and director of CHI. “With Yingzi’s expertise, we are poised to take advantage of opportunities in the field to advance our understanding of immune-mediated diseases impacted by the bacterial communities that live within us.”