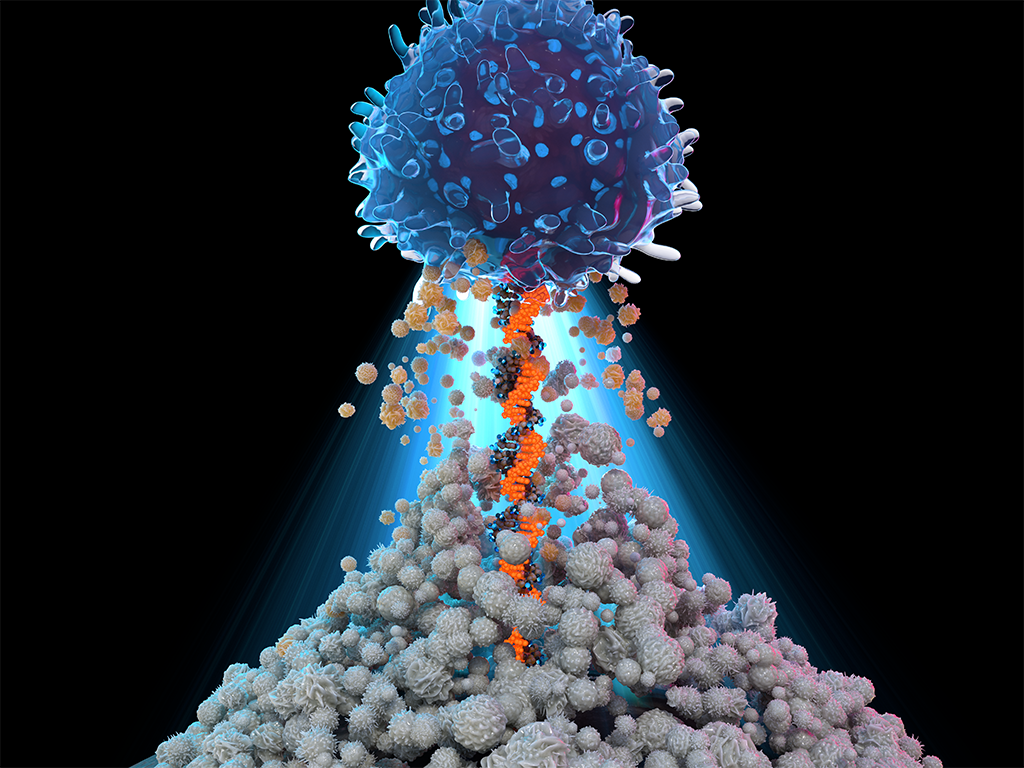
Maximizing the Power of T-cells
Northwestern Medicine investigators are steering CAR T-cell therapy research and treatment development to improve survival and quality of life for patients with cancer.
By Melissa Rohman
In 1988, scientists led by Steven A. Rosenberg, MD, PhD, chief of Surgery at the National Cancer Institute, developed a new immunotherapy involving tumor infiltrating lymphocytes in which white blood cells were taken directly from a patient’s tumor, grown in large numbers in a lab, and then given back to the patient. The novel therapy, detailed in a breakthrough study published then in The New England Journal of Medicine, showed for the first time how this innovative approach could effectively target and fight cancer.
This discovery would ultimately lay the groundwork for the development of many present-day immunotherapies, including CAR T-cell therapies, and ultimately inspire the establishment of robust CAR T-cell therapy research and clinical programs, such as the Robert H. Lurie Comprehensive Cancer Center‘s program at Northwestern Medicine.
Today, CAR T-cell therapy is most used to treat lymphomas — cancers that form in the lymphatic system — including diffuse large B-cell lymphoma, an aggressive form of B-cell lymphoma. CAR T-cell therapy is also used to treat multiple myeloma, a cancer of plasma cells, and acute lymphoblastic leukemia (ALL), in which bone marrow produces too many lymphocytes and can spread to other organs.
In 2017, the FDA approved the first CAR T-cell therapy, tisagenlecleucel, for the treatment of pediatric and adult ALL. There are now a number of CAR T-cell therapies approved by the FDA for the treatment of blood cancers — approvals which, in large part, have been made possible by the work of Northwestern Medicine’s CAR T-cell Therapy Program. The initial clinical trials of CAR T-cell therapy in lymphoma were led by Lurie Cancer Center physician-scientists, Leo Gordon, MD, the Abby and John Friend Professor of Oncology Research and professor of Medicine in the Division of Hematology and Oncology, and Reem Karmali, MD, MS, associate professor of Medicine in the Division of Hematology and Oncology.
The goal of the CAR T-cell therapy program is to use innovative therapies and treatment strategies, which include CAR T-cell therapy, to treat and ultimately cure people diagnosed with blood cancers, including lymphomas.

“The goals of the program are to think outside the box and use treatments that can better target the biology of the cancer and impact the overall survival of patients,” Karmali says. “Everything that we do should be and is geared towards improving outcomes for patients, be it lifespan or side effects or quality of life.”
With expanded research across the Northwestern Medicine system, the program provides robust clinical care and leads various clinical trials studying next generation CAR T-cell therapies. In addition, it is integrated with Ann & Robert H. Lurie Children’s Hospital of Chicago, where CAR T-cell therapy is administered to pediatric patients with B-acute lymphoblastic leukemia. Lurie Cancer Center’s Sarcoma Program, led by Seth Pollack, MD, the Steven T. Rosen, MD, Professor of Cancer Biology and professor of Medicine in Hematology and Oncology, is also testing CAR T-cell therapies in patients with sarcoma.
“Where we are today in terms of availability to patients is because of some of the work that Northwestern has done and participated in terms of clinical trials,” Karmali affirms.
MOVING TO THE FRONT LINE
The standard of care for patients with B-cell lymphoma includes chemoimmunotherapy, which is currently effective in only 60 percent of patients, according to Karmali. In the other 40 percent of patients, cancer recurrence will occur, and patients will need a stem cell or bone marrow transplant. The treatment, however, is toxic and not all patients will respond well to treatment.
“For many people, often the goal was to really just control the disease as best as we could, but not really achieve a cure,” Karmali says.
Enter CAR T-cell therapy. For patients who didn’t qualify for a stem cell transplant, Northwestern-led clinical trials allowed many of these patients to undergo CAR T-cell therapy in lieu of a stem cell transplant, extending patient survival and curing many patients, according to Karmali.
The goals of the program are to think outside the box and use treatments that can better target the biology of the cancer and impact the overall survival of patients. Everything that we do should be and is geared towards improving outcomes for patients, be it lifespan or side effects or quality of life.
Reem Karmali, MD, MS
Thanks to additional clinical trials, CAR T-cell therapy is now the standard of care for patients with recurrent cancer who don’t respond to first-line chemoimmunotherapy.
“CAR T and other cellular therapies may in fact one day replace stem cell transplant in lymphoma, myeloma, and certain leukemias,” Gordon explains. “We are not there yet, but CAR T therapy and other cellular therapies are a more targeted form of allogeneic stem cell transplant, which in fact is the ‘first’ cellular therapy.”
TARGETING SOLID TUMORS
While CAR T-cell therapy has proved effective in patients with hematologic cancers, it currently remains ineffective in treating solid tumors. The reasons why are not yet clear, however possible answers loom within the field, according to Leonidas Platanias, MD, PhD, director of Robert H. Lurie Comprehensive Cancer Center, Jesse, Sara, Andrew, Abigail, Benjamin and Elizabeth Lurie Professor of Oncology, and professor of Medicine.
“For myeloid tumors it’s because there are what we call myeloid suppressor cells — cells that suppress in the environment of some myeloid cells. In solid tumors, it’s a little different and that may be that the cells don’t get access within the tumor,” Platanias says.
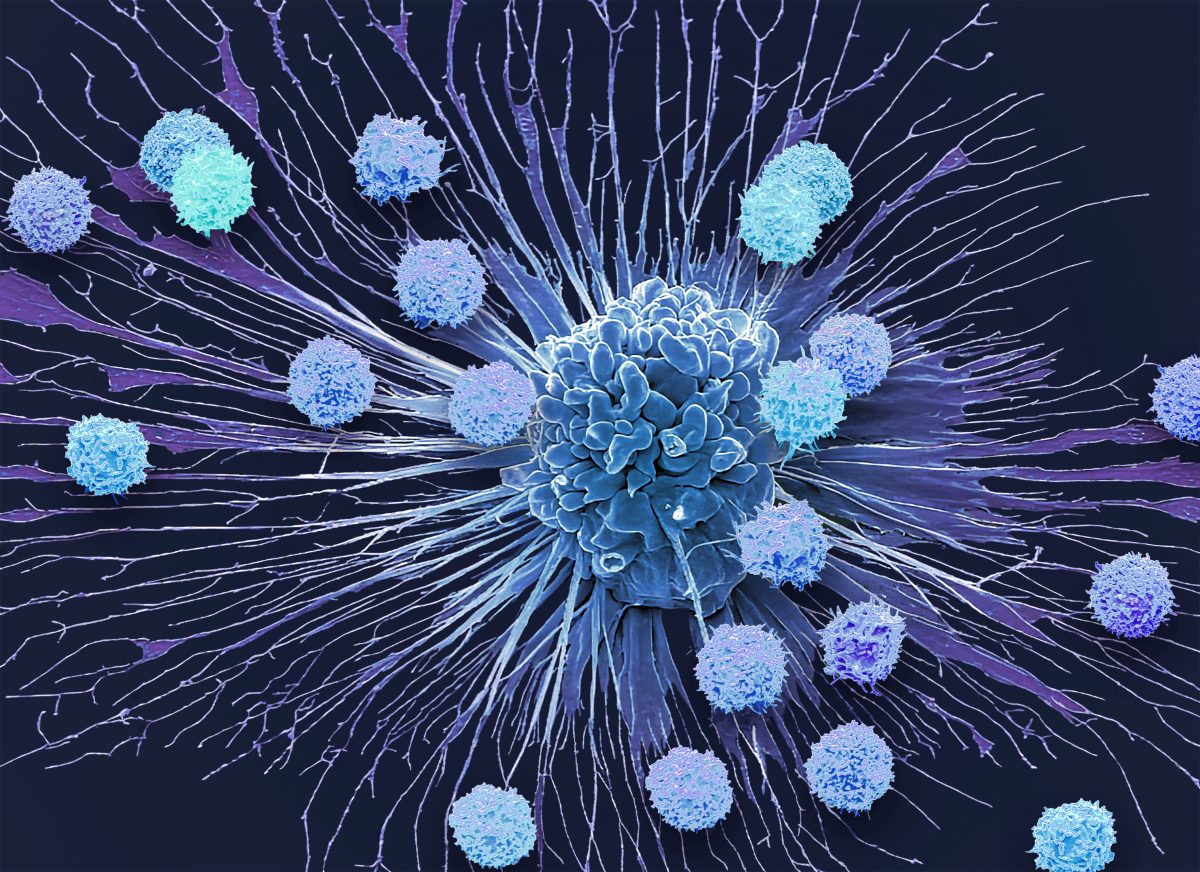
A recent breakthrough study led by Lurie Cancer Center member Jaehyuk Choi, MD, PhD, associate professor of Dermatology and of Biochemistry and Molecular Genetics, found that inserting a gene encoding a unique mutation in T-cells that cause lymphoma into normal human T-cells made them 100 times more potent at killing cancer cells without any indication of becoming toxic.
A collaboration between Northwestern and the University of California San Francisco (UCSF), the study published in Nature demonstrated that the engineered T-cells were able to kill tumors derived from skin, lung, and stomach in mice, suggesting a potential strategy for effectively targeting solid tumors without added toxicity.
“We used nature’s roadmap to make better T-cell therapies,” Choi says. “The superpower that makes cancer cells so strong can be transferred into T-cell therapies to make them powerful enough to eliminate what were once incurable cancers.”
TACKLING CHALLENGES AND LOOKING AHEAD
Karmali is currently leading clinical trials that aim to determine whether CAR T-cell therapy is more effective than standard chemoimmunotherapy in high-risk patients as first-line treatment. Other ongoing research efforts involve using novel CAR T products that target different proteins on the cell surface.
“We may be heading towards a one-and-done treatment that’s much quicker, that’s perhaps more effective, and in some instances even better tolerated than six cycles of intensive chemoimmunotherapy,” Karmali states. Positive outcomes with CAR T-cell therapy are also dependent on patient accessibility, especially for patients living in rural and underserved areas, and patient education, Karmali emphasizes.
“There are some unique side effects associated with CAR T, and so one really needs to be accustomed to recognizing and dealing with these side effects, and that really only comes with being in it and dealing with these constructs,” Karmali says.
Side effects typically occur within the first two weeks of receiving CAR T-cell therapy and can include cytokine release syndrome — an inflammatory syndrome characterized by fever and multiple organ dysfunction — and immune effector cell associated neurologic syndrome, or ICANS, which can cause tremors, aphasia, confusion, and, in some cases, seizures. In January, the FDA also issued a call to add a class-wide boxed warning to six commercially available CAR T therapies to inform patients and providers of their potential risk of secondary T-cell malignancies.
Nevertheless, Karmali says it’s important to affirm to patients that “the risk is worth the reward” in terms of pursuing the therapy and figuring out how to get to and be near their chosen medical institution to receive continuous care and observation.
Patient accessibility is also key to having more diverse clinical trials and improving health equity, Karmali maintains.
“A lot of what we’re trying to move towards is really improving accessibility and the diversity of patients that are included in our studies so that we have a better sense of how we can use this type of therapeutic in a more diverse population that’s more representative of the U.S.,” she says.
In addition to robust clinical programs and clinical care, the development of advanced molecular technologies in the last few decades has established a bright future for CAR T-cell therapy research and therapeutic development.
“We now have very sophisticated molecular techniques and capacity to do many more things using modern molecular biology and bioengineering, which is something that Northwestern likes to do,” Platanias says. “So hopefully we will see major breakthroughs in the future and much more impactful outcomes.”










