Turning Back the Clock
A new longitudinal study within the Human Longevity Laboratory investigates aging, with the ultimate goal of finding ways to reverse its negative effects.
By Emily Ayshford

Some physical aspects of aging seem unavoidable: eyesight worsens, hearing degrades, and gaits slow.
But other indicators are hidden — DNA methylation biomarkers change, for example, while the sugar structures circulating within our blood shift to become abnormal. Other more elusive clues can only be found when scientists or artificial intelligence (AI) programs analyze test results, like EKGs, for signs of aging.
Today, scientists can use data and testing to determine a person’s “biological age” rather than chronological age, and potentially leverage interventions to slow or even reverse aging.
By investigating the relationship between chronological age and biological age across different organ systems, faculty at the new Human Longevity Laboratory at Northwestern University Feinberg School of Medicine aim to provide knowledge and insight to help scientists develop methods to extend the human lifespan.
As part of Feinberg’s Potocsnak Longevity Institute, a team led by Douglas Vaughan, MD, director of Potocsnak Longevity Institute, has launched a longitudinal, cross-sectional study to investigate aging across different organ systems. The team will then use that information to test interventions that might reverse or slow down the process of aging.
“The biology of aging is rapidly becoming demystified,” says Vaughan, who also serves as the Irving S. Cutter Professor of Medicine Emeritus. “And our ability to measure biological age is real. We’re in a unique moment in human history where we might be able to do something about aging and ensure that everyone has a better chance at a healthier life.”
AN ARRAY OF TESTS THAT DETERMINE BIOLOGICAL AGE
In fact, the goal of the lab is not to extend life span. It aims to extend “health span” — the length of time that a person is healthy — especially for people who are disadvantaged from an aging standpoint.
That includes people who have a higher burden of exposure to adverse social determinants of health and people living with chronic HIV infections.
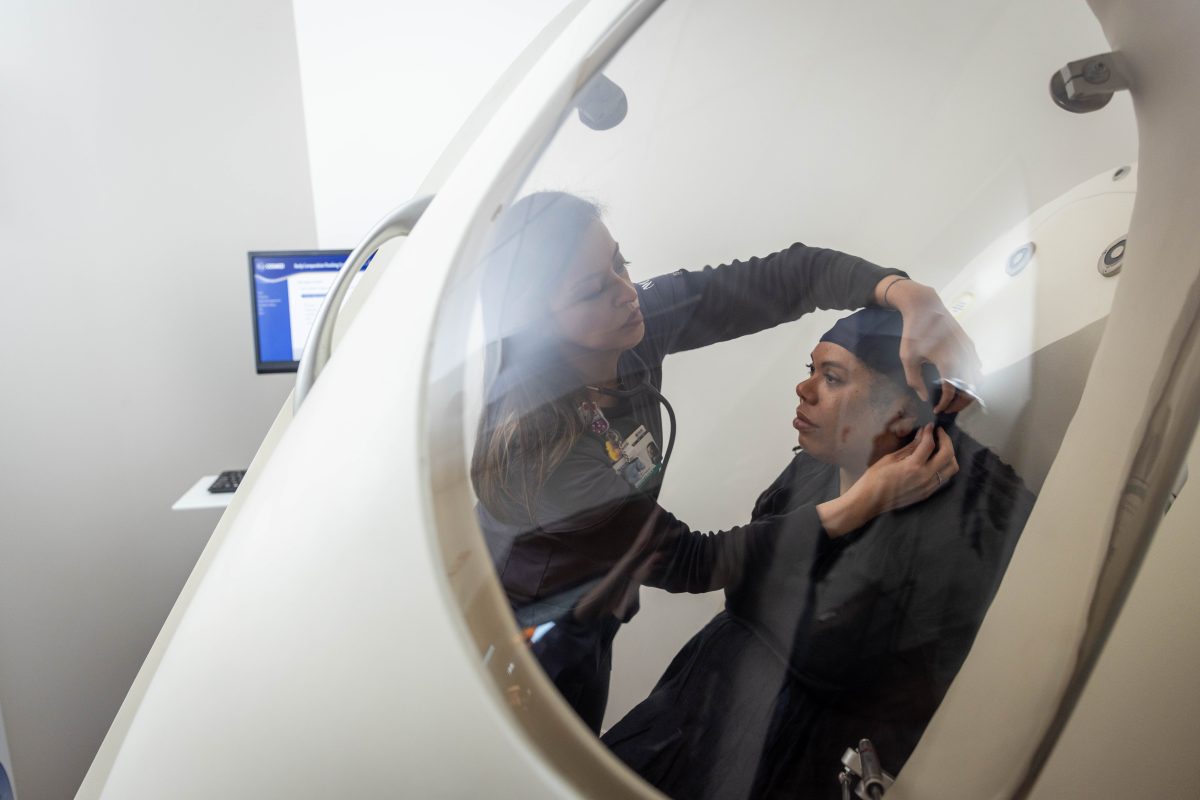
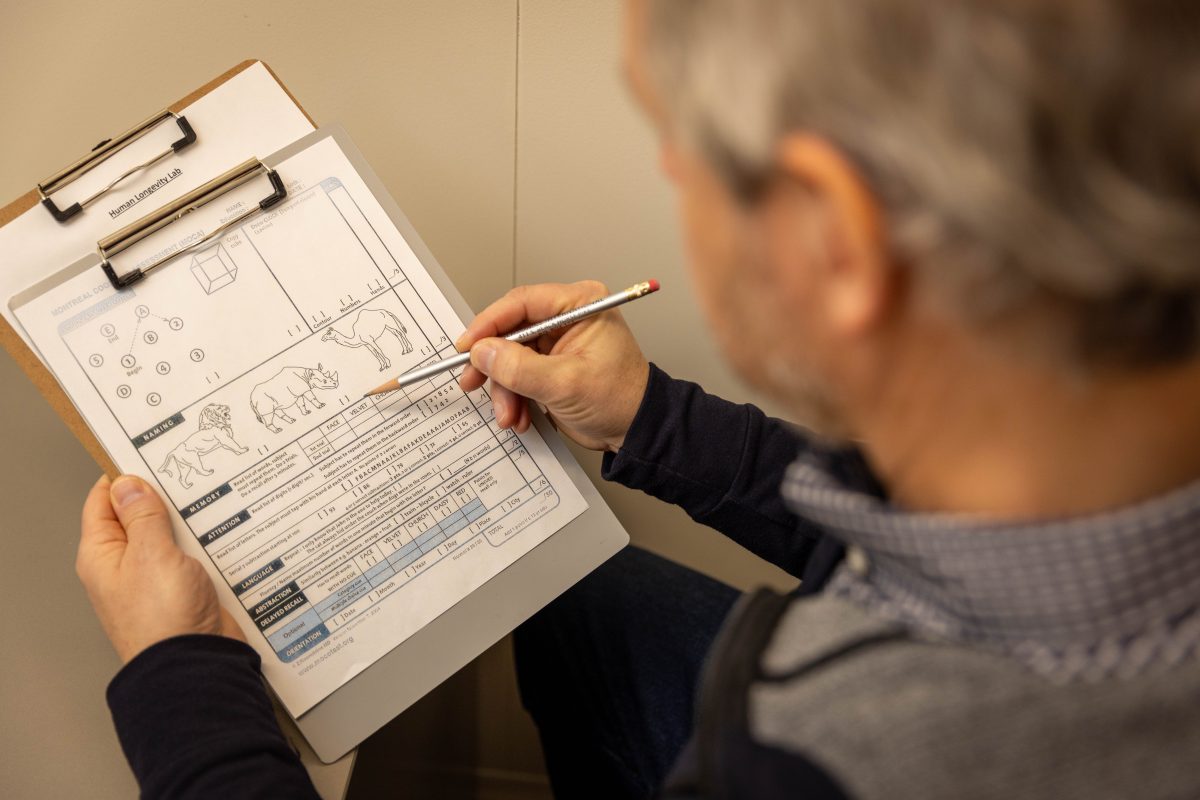
But first, faculty must understand aging across a wide variety of the population. To do so, the lab is recruiting and enrolling up to 500 participants over the next year to undergo a variety of aging tests. These include tests of physiological function, including hearing and smell tests, and measures of physical ability, such as grip strength tests and gait assessments. Participants even get their turn in a futuristic-looking capsule called the BodPod, which measures the ratio of their body’s fatty mass to lean mass.
Cardiovascular health is measured through EKGs and heart-rate tests, as well as through retinal imaging, where the health of blood vessels can be studied. Finally, participants have their biological age measured through DNA methylation, a measure of modifications in their DNA. When compounds called methyl groups attach to DNA in certain locations, it can be a biomarker of accelerated aging.
Participants are given a report on their overall biological age, but one number might not reveal everything. Aging can differ across a person’s organ systems, and it may well vary over short timespans.
And not all measures are created equal — as investigators continue the study, they hope to eliminate measurements that aren’t as relevant to aging and bring on new tools that could offer more insight.
HARNESSING THE POWER OF AI
One of those tools is AI, overseen at the lab by Baljash Cheema, ’15 MD, ’20 MSCI, ’22 MSAI, assistant professor of Medicine and transplant cardiologist at Northwestern Medicine. Cheema is a cardiologist who also has a Master of Science in AI degree from Northwestern University McCormick School of Engineering. He is keen on using machine learning technology in medicine.
“AI is really good at specific tasks, like looking at 10 million echocardiograms and predicting one parameter,” he says. “So we wanted to incorporate this ability into the study of aging.”
The biology of aging is rapidly becoming demystified. And our ability to measure biological age is real. We’re in a unique moment in human history where we might be able to do something about aging and ensure that everyone has a better chance at a healthier life.
Douglas Vaughan, MD

Established in 2022, the Potocsnak Longevity Institute, which includes the Human Longevity Lab (HLL), is a pioneering initiative that delves into the science of aging through various specialized centers. (Photo credit: Teresa Crawford)
Currently, the lab has integrated AI tools already available on the market. Faculty work with a group in Brazil that has trained an AI model to predict someone’s age based on their EKG results. “What’s fascinating is that if the AI model predicts that you’re older than you actually are, that corresponds with you having some degree of cardiovascular risk,” Cheema says.
The team also works with a group in New Zealand that has trained an AI model to predict someone’s age based on retinal images. Because it is the only place where physicians can image blood vessels, it provides information on blood vessels’ width and twist. “That’s another window into cardiovascular health,” Cheema says.
Another AI collaboration lies closer to home. To analyze the speed and movement of a participant’s gait, the lab works with James Cotton, MD, PhD, assistant professor of Physical Medicine and Rehabilitation and a physician at Shirley Ryan AbilityLab. Cotton’s AI tech analyzes joint movement, speed, and quality of walking, and compares it to that of people around the same age, offering a muscular-skeleton component of biological age.
In fact, almost all of the lab’s tests have some AI aspect built into them. “I think AI will be a big driver in what we learn,” Vaughan says. “And when we have a great dataset of participants of all different ages, we can use AI to analyze that to give us a multidimensional composite of biological age.”
The lab’s first year will focus on measuring how much aging varies across people, organ systems, and time. (Some participants will be invited back to be reassessed after a few months just to check how time affects the aging process.)


IDENTIFYING INTERVENTIONS THAT WORK
Then, lab members hope to quickly pivot to testing interventions that could potentially slow or reverse aging. That will involve recruiting participants into randomized controlled trials to test therapies like metformin, which helps control blood sugar and has been shown to potentially slow aging. Trials could also include lifestyle changes, such as intermittent fasting, caloric restriction, and even meditation.
“There is a lot of misinformation out there on what slows aging,” Vaughan says. “We want to start with a healthy dose of skepticism that anything works. We are going to be the lab that tests these interventions rigorously and without bias.”
The ultimate goal is to “bend the curve” of aging, says John Wilkins, MD, ’11 MSCI, associate director of the Human Longevity Lab and associate professor of Medicine and of Preventative Medicine. “We’re going to test interventions that have already been proved to be safe and effective,” he says. “We don’t yet know which will work the best, but science isn’t fun when you know the answer. If we find an answer, it will help people live healthier, longer lives — particularly those who are disadvantaged. We want them to live the longest, healthiest life possible.”
CREATING A GLOBAL NETWORK
Though the lab hopes to get a database of hundreds of participants in the Chicago area, faculty do not want to stop there. Lab leadership is already in talks with research groups around the world to create a network of similar labs, with Northwestern as the flagship site. Potential sites have already been identified in Asia, South America, Europe, and Africa.
A global network would allow more data collection and more testing, especially among a wide variety of populations.
“What differentiates the Human Longevity Lab is our dedication to multifactorial measurement of aging,” Vaughan says. “It’s our use of artificial intelligence, and our talented, thoughtful faculty who bring their expertise to the table. We have the ability to bring this all together and hopefully increase the health span for many people.”
EXPLORE MORE
Take a look inside the Potocsnak Longevity Institute’s Human Longevity Laboratory.
Listen to John Wilkins, MD, associate director of the Human Longevity Laboratory at the Potocsnak Longevity Institute, discuss the Human Longevity Lab’s longitudinal cross-sectional study.










