Science at Work
Investigators tackle the pandemic from all sides.
Science at Work
Investigators tackle the pandemic from all sides.
The COVID-19 response at Feinberg was fast and multifaceted. As of press time, more than 230 projects were in motion, from interventional studies and data analytics to discovery, diagnostics, and specimen testing.
“We aimed to maximize our research impact and minimize intrusions on critical healthcare pathways,” says Rex Chisholm, PhD, the Adam and Richard T. Lind Professor of Medical Genetics and vice dean for scientific affairs and graduate education.

A beautiful target
Some of the most critical work — identifying potential drug targets — started in mid-January, when Karla Satchell, PhD, professor of Microbiology-Immunology and director of the Center for Structural Genomics of Infectious Diseases (CSGID), began leading a multi-institution, international effort to investigate the structure of the novel coronavirus. By rebooting previous research related to SARS, the center was quickly able to begin investigating the protein structures of the virus with the goal of finding new drug targets for COVID-19.
Scientists mapped the atomic structure of two critical proteins in a complex, nsp10/nsp16. These proteins modify the genetic material of the virus to make it look more like the host (human) cell RNA. This allows the virus to hide from the cells, giving it time to multiply. If a drug can be developed to inhibit nsp10/nsp16, the immune system should be able to detect the virus and eradicate it faster.
“This is a really beautiful target, because it’s a protein absolutely essential for the virus to replicate,” says Satchell.

The structure of nsp10/nsp16 was released to the scientific community March 18 on the RCSB Protein Data Bank. This was the fourth protein structure of a potential drug target of SARS-CoV-2 determined by the CSGID team of scientists. The center is racing to release more structures for drug development.
“We need multiple drugs to treat this virus, because this disease is likely to be with us for a long time,” says Satchell. “It’s not good enough for us to develop a single drug. If COVID-19 develops a resistance to one drug, then we need others.”
“It’s been amazing to see the sharing of resources. It used to be that if you had a new drug target, the first thing you did is kept it quiet,” she added. “Now people are making a lot of information public, and that is a great blueprint for the community to follow, not only for this but for the future.”

Providing Support and Resources
In response to the pandemic, the open, crowdsourced Chicago COVID-19 Resource Repository was created by Feinberg faculty and staff in the Center for Community Health’s Alliance for Research in Chicagoland Communities (ARCC) program, which has presence in the Institute for Public Health and Medicine (IPHAM) and the Northwestern University Clinical and Translational Sciences Institute (NUCATS).
The repository offers lists of resources for physical and mental health, housing, food, financial and legal services, substance use disorder services, internet access, childcare, education, volunteer opportunities, donations, and more. IPHAM also coordinated the Chicago COVID-19 Coalition, which involves faculty, staff, and trainees across multiple Chicago-area academic centers, state and city health departments, numerous regional health systems, and other stakeholders.
“The COVID-19 epidemic has ignited a vigorous groundswell of selfless collaboration,” says Ron Ackermann, MD, MPH, director of IPHAM and senior associate dean for public health.
As COVID-19 began to spread, the NUCATS Institute’s agility helped better position researchers in their pursuit to translate novel investigations into meaningful solutions. Initiatives and support included:
- Rapid response grant funding (more details here)
- Help garnering supplemental research funding for researchers from national agencies
- Launching The New Normal, a Chicago-based clinical research portal
- Led by director Richard D’Aquila, instituting a feasibility review, a critical step in ensuring Northwestern was equipped to complete research projects being proposed
- Adapting clinical research unit to conduct clinical trials
“NUCATS, and the NIH’s National Center for Advancing Translational Science that funds the Institute, have made responding to the emergency of this pandemic the highest priority,” says Richard D’Aquila, MD, director of NUCATS, senior associate dean for clinical and translational research and associate vice president of research. “Our research teams have already made many contributions, and we are committed to helping them continue and grow those efforts.”
A testing lab in 10 days
As soon as the U.S. Food and Drug Administration allowed certain laboratories to develop diagnostic tests for coronavirus, Northwestern Medicine and Feinberg began working together to increase the healthcare system’s testing capacity from about 90 per day to more than 360 per day — and in the process, greatly reducing test result turnaround times.
Staff from NUSeq Core Facility in the Center for Genetic Medicine picked up patient samples from the hospital and brought them to NUSeq for testing, using the facility’s real-time quantitative polymerase chain reaction machines. The data was then sent back to the health system for analysis and reporting. Six Feinberg research staff members began working in shifts around the clock to more than quadruple Northwestern Memorial Hospital’s testing capacity.
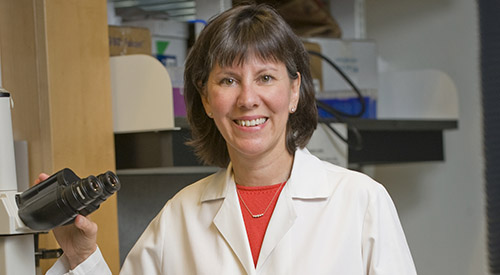
“These steps all came together over about 10 days, including two weekends — a remarkable feat!” says Xinkun Wang, PhD, director of NUSeq and research associate professor of Biochemistry and Molecular Genetics. Wang led this effort, along with Elizabeth McNally, MD, PhD, the Elizabeth J. Ward Professor of Genetic Medicine, professor of Medicine in the Division of Cardiology, and director of CGM.
“Our research staff routinely performs the exact same steps as those used in the COVID-19 virus tests, and our research labs have the necessary machines for this type of analysis,” says McNally. “It really became a question of how quickly we could get the proper certifications and training in place. Luckily, we have fantastic research staff who worked seamlessly with the Northwestern Medicine clinical lab to make this all happen. It took a lot of lifting, but it got done and we are now helping reduce the backlog and hopefully will be able to ramp up capacity even more than projected.”
In addition to joining forces with Feinberg’s NUSeq Core Facility, Northwestern Medicine is testing in-house for COVID-19 in three other platforms.
COVID-19 and African Americans
In April, Clyde Yancy, MD, MSc, vice dean for Diversity and Inclusion and chief of Cardiology in the Department of Medicine, published an editorial in JAMA shedding light on the glaring disparities in COVID-19 fatality rates. “Persons who are African American or Black are contracting SARS-CoV-2 at higher rates and are more likely to die. Why is this uniquely important to me? I am an academic cardiologist; I study healthcare disparities; and I am a Black man,” he writes.
Yancy, who is the Magerstadt Professor and professor of Medicine in the Division of Cardiology and of Medical Social Sciences, cited data from multiple cities in the U.S., including Chicago, where more than 50 percent of COVID-19 cases and nearly 70 percent of COVID-19 deaths involve Black individuals, although they make up only 30 percent of the population.
He also writes that data have not fully been adjusted for comorbidities. “But concerns go beyond these comorbidities,” he points out. “Where and how Black individuals live matters.” Social distancing is not an option for people living in dense, poor communities and who can’t do their work from home.
“This is a moment of ethical reckoning,” he goes on. “The scourge of COVID-19 will end, but healthcare disparities will persist.”

An antibody test requiring a single drop of blood
As antibody testing ramps up across the country, Northwestern investigators have developed a new method for testing for SARS-CoV-2 (the virus that causes COVID-19) antibodies. The method requires only a single drop of blood collected from a simple finger prick.
A team of Northwestern scientists, including McNally and biological anthropologist Thomas McDade, PhD, together with Feinberg pharmacologist Alexis Demonbreun, PhD, and investigators Richard D’Aquila, MD, associate vice president of research and the Howard Taylor Ricketts, MD, Professor of Medicine in the Division of Infectious Diseases, and Brian Mustanski, PhD, professor of Medical Social Sciences and of Psychiatry and Behavioral Sciences, reported this new test in a paper on MedRxiv, the preprint server for health sciences.
Antibody tests are useful for determining prior exposure to a virus, like the one that causes COVID-19. But current approaches to antibody testing have significant limitations: Point-of-care tests using finger stick blood are qualitative and often inaccurate, while more precise lab-based tests require venous blood. The Northwestern team has developed an approach that combines the convenience of finger stick blood sampling in the home with the analytical rigor that can be applied in the lab.
According to McNally, “Widespread serological testing is essential for figuring out how the virus is spreading in the community, but it is very hard to screen large numbers of people when the tests require people to come to a healthcare provider.”

A Wearable Device for Tracking Symptoms
John Rogers, PhD, the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering, and Neurological Surgery, collaborated with the Shirley Ryan AbilityLab to develop a novel wearable device and create a set of data algorithms specifically tailored to catch early signs and symptoms associated with COVID-19 and to monitor patients as the illness progresses.
Capable of being worn 24/7, the postage-stamp-size device produces continuous streams of data and uses artificial intelligence to uncover subtle, but potentially life-saving, insights. In the coming weeks, the Northwestern and AbilityLab teams will continue collecting patient data to strengthen their algorithms — through deployments both in the clinic and at home.
The critical importance of basic science
From the earliest weeks of the COVID-19 pandemic, scientists across Northwestern mobilized to understand the virus and find a treatment for it. Using next-generation sequencing technology that was unfathomable just 15 years ago, scientists quickly developed a picture of the virus’ genetic structure, providing a framework for developing vaccines, therapies, and tests.
This is a reminder of the importance of basic molecular science, something summarized profoundly by Ali Shilatifard, PhD, the Robert Francis Furchgott Professor and chair of Biochemistry and Molecular Genetics, director of the Simpson Querrey Center for Epigenetics, and professor of Pediatrics, in a recent editorial in Science Advances, where he also serves as editor.
“A pandemic — especially one caused by a mysterious or newly discovered infectious agent — engenders a stark reminder that supporting fundamental research has been a prudent investment of public funds,” he wrote. Now more than ever, the health of our society depends on the understanding of the molecular basis of human disease.
A pandemic — especially one caused by a mysterious or newly discovered infectious agent — engenders a stark reminder that supporting fundamental research has been a prudent investment of public funds.
Ali Shilatifard, PhD
Straight Talk
From the emergence of the novel coronavirus as a deadly threat in Wuhan, China, Robert Murphy, MD, executive director of the Institute for Global Health and director of the Center for Global Communicable Diseases, warned of its spread. On March 24, he outlined the best way forward (in bold print below).
Reflecting on these guidelines in late June, Murphy said, “I’m really stunned at my statements from March because at the time, I was heavily criticized for being an alarmist. But I stood firm, and looking back, I stand by each and every one of those points.” He then accessed and graded each response (text following bold print).
- Keep schools and universities closed. This was a very smart idea and alone prevented hundreds of thousands of new infections and many deaths. Grade: A
- Ramp up testing and test healthcare workers. Another great idea that couldn’t really be done because we had such poor testing capacity back then. It is clear now just how important testing has become. We can’t control the epidemic without knowing who and how many are infected. Testing will have to increase even more as we move toward opening up the whole economy, maybe by as much as 10-20 fold. I’m part of a program referred to as Rapid Acceleration of Diagnostic Testing for Coronavirus-19, or RADx, funded by the NIH. We are accelerating novel diagnostic tests that are easier, faster, and less expensive than standard tests. As for healthcare workers, it looks like about 4 percent got infected on the job. The rate has diminished as the PPE capacity increased, number of patients decreased in most places but not all, and proper infection control procedures were put into place. Grade: C-
- Increase production of hospital supplies and capacity, using the Defense Production Act (DPA) if necessary. Our haphazard response continues to stumble along. While improvements have been made, the path has been bumpy. At least now we have identified one of the weakest links in our public health defense system. This will require a complete overhaul of our public health readiness program. Grade C-
- Invest in massive vaccine and antiviral drug development initiatives. Here the public and private sectors globally have succeeded. Amazingly, The Oxford Vaccine Group has a promising vaccine candidate that is already entering Phase III clinical trials. If successful, there could be access to this vaccine as early as September 2020. So, if you live in the United Kingdom, you may get lucky. Twelve other vaccines have begun human trials, and over 100 others are in the pre-clinical phase. Things look promising on this front. As for new drugs, remdesivir was approved for use in very ill patients and more drugs are on the way. An old drug, the steroid dexamethasone, was shown to improve survival in critically ill patients. All good news here, but we need more, including drugs you would take right after being diagnosed, essentially a “test and treat” strategy that would prevent severe complications and decrease transmission rates at the same time. Grade: A
- Support the unemployed with funding and health insurance. We have been unsuccessful in this regard with only limited support for most of the workers. The pandemic has exposed our shambolic health care system for what it really is. Grade: F
- Vigilantly enforce public health policies such as social distancing. Our public health national leadership has been for the most part compromised on this issue, with most decisions left to the states. The policies are inconsistent and have become unnecessarily politicized. States that are more vigorously enforcing social distancing and wearing of masks have done better than those that have not. The country as a whole now has the most documented cases and deaths worldwide. Our new case rate is so high now (107/100,000 population), that Americans are very likely to banned from travel to Europe. Of the major countries, only Brazil is worse than the US with a rate of 190/100,000. Grade: D-