Tracing Back
Feinberg scientists get to the genetic roots of epilepsy to tackle this common and life-altering disorder.
by Cheryl SooHoo
Photography by Gr8y Productions and Teresa Crawford
Epilepsy, with its unpredictable seizures, threatens the lives and quality of life for as many as one percent of the world’s population. Misfiring brain neurons are the hallmark of the neurological disorder that occurs for myriad reasons — from head trauma to infection — with genetic mutations being another key driver. Only in recent years has genetic testing become the standard of care, accelerating research aimed at better understanding the genetic etiology of the disease to develop more effective, if not curative, therapies.
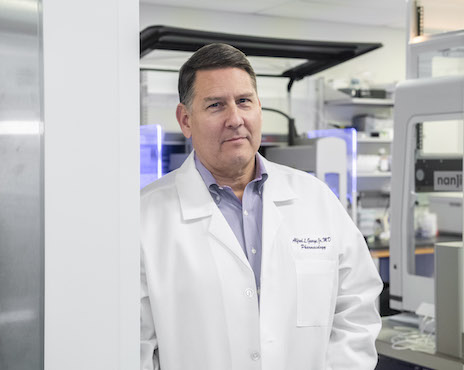
“The evidence continues to mount that the causes of epilepsy are rooted in the genetics of brain development,” says Alfred L. George Jr., MD, the Alfred Newton Richards Professor and chair of Pharmacology and director of the interdisciplinary, multi-institutional Channelopathy-Associated Epilepsy Research Center, funded by the National Institutes of Health’s (NIH) Centers Without Walls initiative. “It seems likely that common forms of epilepsy occur because of genetic variation in many genes, whereas less common, yet often more severe, forms of the disease can be traced to mutations in single genes.”
Northwestern Medicine is one of the few places in the country where a critical mass of investigators studies the genetic underpinnings of epilepsy in both children and adults. Collaborating with epileptologists caring for patients at Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern Memorial Hospital, Feinberg research teams have extraordinary access to the invaluable clinical information needed to translate new breakthrough therapies into 21st century care.
Pinpointing early-onset epilepsy genes
When it comes to epilepsy, the gene KCNQ2 strikes early. A newborn who experiences an obviously unexplainable seizure within 48 hours of life has a better-than-average chance of having a KCNQ2 genetic mutation. Encoding a neuronal potassium channel, KCNQ2 controls electrical activity in the brain. KCNQ2 is one of the most frequently found genes associated with neonatal epilepsy. While seizures may resolve within the first year for some children who go on to develop normally, others have persistent seizures that can severely impact their cognition, communication, and physical function.
In 1998, two separate U.S. and European research teams simultaneously identified KCNQ2 and its connection to early-life monogenetic, or single-gene causing, epilepsies. Since that time, increased genetic testing uncovers more and more individuals with KCNQ2-related epilepsies. The significance of this gene did not escape the attention of George and key collaborators at Lurie Children’s and elsewhere when establishing the Channelopathy-Associated Epilepsy Research Center in 2018. KCNQ2 was one of the first genes tackled by the center, which is supported by a five-year $12 million grant from the NIH that began in 2018.
“Another important aspect of studying KCNQ2 was the existence of an FDA-approved drug called retigabine that boosts the activity of the ion channel encoded by this gene,” George adds. “We studied a large number of KCNQ2 mutations to understand their functional consequences, while also examining which ones were amenable to treatment with this drug.”

KCNQ2 variants associated with early onset epilepsy number in the hundreds for this single gene. Many laboratories have limited capacity to study more than a handful of genetic mutations at a time, making progress painfully slow for families pleading for more effective therapies for their children. Fortunately, Feinberg’s Department of Pharmacology houses an automated electrophysiology platform for high-throughput drug screening of ion channels — sophisticated equipment typically found in the pharmaceutical industry. In the February 2022 issue of JCI Insight, George and his team published their work using this technology to study the effect of retigabine on a record-breaking 80 variants of KCNQ2. This unprecedented large-scale evaluation revealed that not all KCNQ2 mutations respond the same way to retigabine and that may have implications for identifying which patients will most benefit from the drug and possibly other similarly acting drugs currently in development.
Other KCNQ2 discoveries at Northwestern have catalyzed new directions for developing novel therapies. In a study published in the February 2021 issue of eLife, Feinberg investigators for the first time characterized how a KCNQ2 variant affects human neuronal activity in a “dish.” The scientists used patient-derived neuron models originated in the laboratory of Evangelos Kiskinis, PhD, assistant professor of Neurology in the Division of Neuromuscular Disease in the Ken and Ruth Davee Department of Neurology, to examine the impact of KCNQ2 mutations. The KCNQ2-specific models exhibited electrophysiology activity — a burst-suppression activity model — similar to patterns seen in the electroencephalograms of children with KCNQ2 epilepsy.
This work further inspired Kiskinis, George, and other collaborators to develop customized therapeutic molecules to target KCNQ2. The team’s gene therapy approach employs a modified RNA technology called antisense oligonucleotides (ASOs). The gene-modulating ability of ASOs offers a viable, more personalized option for treating uncommon diseases like genetic epilepsies. In recent years, RNA therapeutics have proven successful in treating spinal muscular atrophy — a rare neuromuscular disorder that was once universally fatal. Currently, no ASO therapeutic exists for treating pediatric epilepsy, but based on preliminary data from a proof-of-concept study completed last year, Feinberg investigators are hopeful.
Focus on Adults with Epilepsy
The past 20 years has seen an exponential growth in our understanding of the genetics of epilepsy. A decade ago, about five genes were known to cause the disorder. Today, hundreds of genes associated with epilepsy have been identified, offering a launching pad for developing new treatments not only for children, but also those who have grown up with or begun experiencing seizures sometime during adulthood.
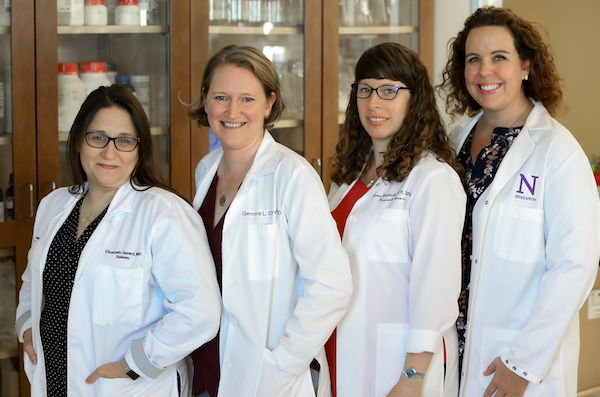
From left to right: Elizabeth Gerard, MD; Gemma Carvill, PhD; clinical research associate Irena Bellinski, RN, MPH; and senior genetic counselor Lisa Kinsley, MS, CGC. Photo by Teresa Crawford.
Machine learning techniques are often limited by their datasets — they must have enough good data to learn from — but the explosion of data and higher-resolution imaging technology within the past several years has begun to lead to new insights in the field.
While most epilepsy research has focused on children, little has been conducted on genetic causes in adult patients. In addition to pediatric epilepsy, Gemma Carvill, PhD, assistant professor of Neurology, of Pediatrics, and of Pharmacology, has carved out a unique niche by investigating genetic variants that can cause the disease in adults. To that end, she partners with Elizabeth Gerard, MD, associate professor of Neurology, in directing the Adult Epilepsy Genetics Translational Research Program at Northwestern Memorial Hospital — one of just a few programs of its kind in the country.
An NIH New Innovator Award recipient, Carvill received a $1.5 million five-year grant in 2018 to support her work. In the area of adult epilepsy, some of the variants identified by the Carvill lab occur in genes of the mTOR pathway, which helps promote cell growth and proliferation. In the June issue of Brain, Carvill and colleagues described their discovery of a new method to determine whether individual genetic variants in the epilepsy-associated gene SZT2 cause a neurodevelopmental disorder.
SZT2 variants have been associated with early-onset epilepsy and developmental delays. The gene also plays a role in the mTORC1 signaling pathway. Classifying SZT2 variants as benign or pathogenic has been a challenge due to the large size of SZT2, which contains more than 3,400 amino acids. Using CRISPR-Cas9 genome editing and next-generation sequencing, the team developed a rapid assay to ultimately reclassify a recurrent variant as pathogenic and determine that it is also a founder variant prevalent in individuals of Ashkenazi Jewish ancestry. This finding has implications for including the variant in targeted prenatal testing panels and identifying individuals eligible for more tailored therapeutic approaches.
“While identifying the genetic cause of epilepsy is beneficial, the major impact of this work is when it informs clinical care or leads to precision therapies,” says Carvill. “We are always working to take that next step and look for ways to capitalize on discoveries to understand epilepsy, find new treatments, and make a difference in the lives of patients and their families.”
“We demonstrated that we could use our patient-specific stem cell models to screen and validate customized ASO molecules to target specific KCNQ2 mutations,” Kiskinis shares about the study’s early findings. On the basis of these promising results, the team applied this summer for a three-year $1.5 million external grant to further advance this innovative work. “We hope that effective ASO therapies will be able to treat seizures as well as associated comorbidities such as developmental delays,” he adds.

Epilepsy researcher and geneticist Jennifer Kearney, PhD, associate professor of Pharmacology, develops animal models of childhood epilepsy for preclinical evaluation of drug compounds. While KCNQ2 remains an important gene of interest, there are many more epilepsy-linked genes under study at Northwestern. In 2014, Kearney’s team was the first to describe KCNB1 as a new variant involved in the misfiring of neurons, leading to pediatric epileptic seizures. She is currently focusing on a sodium channel gene called SCN2A.
“SCN2A has a very interesting ‘Goldilocks’ effect,” she explains. “Mutations that enhance the gene’s function lead to epilepsy and the ones that inhibit the gene’s function result in disorders on the autism spectrum.” Kearney is developing a mouse model to better understand the function of SCN2A variants and their impact on early-onset epilepsies.
“What’s emerging is the idea that conventional drugs aren’t the only therapeutic weapons at our disposal,” George says. “I’m excited and optimistic about discovering new molecular and genetically-based therapeutic strategies, such as those using RNA, for treating disorders like epilepsy.”
Listen to the Alfred George Breakthroughs podcast
Surgical Care for Seizures

Joshua Rosenow, MD, director of Functional Neurosurgery and professor of Neurosurgery, of Neurology and of Physical Medicine and Rehabilitation
About one third of patients with epilepsy continue to have seizures despite taking multiple medications. But a significant renaissance in epilepsy surgery in the last decade has opened up the possibility of a surgical cure to many patients who were previously not considered surgical candidates, says Joshua Rosenow, MD, director of Functional Neurosurgery. Furthermore, many patients who would have had larger, more invasive procedures can now undergo smaller, minimally invasive procedures with shorter recovery times.
“We can place a small laser fiber directly into the seizure zone through a tiny opening in the skull and destroy it under real-time MRI guidance,” explains Rosenow, who is also a professor of Neurosurgery, of Neurology and of Physical Medicine and Rehabilitation. In this scenario, patients typically only stay in the hospital one night and are back to full activity quickly.
In situations where the area of the brain causing seizures cannot be removed without causing disability, surgeons can now implant electrodes in the affected region. These electrodes are connected to a device mounted in the skull that continuously reads the electrical signals from that area. “We can teach the device to recognize the seizure patterns on the EEG, and the device can deliver stimulation in response to these patterns like a ‘brain defibrillator,’” Rosenow says. He adds that recent improvements in vagus nerve stimulation devices mean that they can also sense a person’s heart rate and deliver extra stimulation if the heart rate increases at the start of a seizure. Finally, not only can responsive neurostimulation therapy significantly reduce seizures, but investigators can acquire valuable insights about a patient’s epilepsy from many hours of EEG recordings.
“We see this as the most exciting time for our specialty and look forward to continuing to help people with chronic neurologic conditions live better lives,” Rosenow says.