by Will Doss
Northwestern’s investment in next-generation sequencing is leading to unprecedented avenues of discovery.
Thirty years ago, the Human Genome Project started, and it took 13 years and nearly $3 billion to complete. Now, thanks to next-generation sequencing (NGS), human genomes can be sequenced in just a few hours for less than $1,000.
“NGS has opened up a new understanding of DNA and chromosome structure, and for human genetics, we are able to sequence many more people and better understand genome variation across individuals and populations,” says Elizabeth McNally, MD, PhD, the Elizabeth J. Ward Professor of Genetic Medicine and director of the Center for Genetic Medicine, which provides full NGS capability to Northwestern.
Recognizing the power of this revolutionary technology, Northwestern has in recent years made a significant investment not only in NGS instruments, but also in the computational analysis of NGS, building a sophisticated infrastructure that according to McNally aids investigators across the research enterprise.
“Every day, investigators around campus are producing and analyzing sequence data,” she says. “And as much data as we generate, we have to analyze it. So we have dedicated about a hundred nodes in Quest — Northwestern’s central computing system — exclusively to genomics analysis.”
At any given time, says McNally, as many as 450 analysts from more than 200 labs are using those nodes, culling NGS data that informs a wide range of studies. “It’s created an enormously wonderful community of people who then can interact and help each other across specialties,” she says.
Supercharging discovery for COVID-19 and beyond
The breakthrough science that NGS has enabled in the past year alone at Northwestern has been remarkable — from the profiling of the three-dimensional genome structure of zebrafish by Feng Yue, PhD, the Duane and Susan Burnham Professor of Molecular Medicine, published in Nature (read more) to a large-scale study about the influence biological sex has on gene expression, led by Barbara Stranger, PhD, associate professor of Pharmacology, published in Science (read more).
NGS has also been a boon for the fast-growing field of epigenetics, according to Ali Shilatifard, PhD, chair of the Department of Biochemistry and Molecular Genetics and the Robert Francis Furchgott Professor of Biochemistry and Molecular Genetics and of Pediatrics. The Shilatifard Lab recently took advantage of NGS and CRISPR screening capabilities to define the role of epigenetic factors in stem cell development and differentiation for a study that was featured in a cover story in Nature Genetics.
But it is NGS’s critical role in COVID-19 research, starting from the earliest days of the pandemic, that has been this powerful tool’s biggest contribution to discovery this year.
“Rapid sequencing of the SARS-CoV-2 RNA genome using NGS immediately provided insight into the singular properties of this coronavirus strain to scientific and clinical communities,” says Shilatifard. “Without NGS, there would not have been a COVID-19 vaccine developed this rapidly today — no way, no how.”
Shilatifard, who is the director of the Simpson Querrey Institute for Epigenetics (SQE), adds that a whole-genome sequencing instrument (acquired by SQE with strategic planning from Northwestern leadership and support from the Simpson Querrey family) provided critical assistance to Northwestern’s Successful Clinical Response in Pneumonia Therapy (SCRIPT) study, published in Nature. Led by co-senior authors Richard Wunderink, MD, professor of Medicine in the Division of Pulmonary and Critical Care, and Scott Budinger, MD, chief of Pulmonary and Critical Care in the Department of Medicine, this was the first study in which scientists analyzed immune cells from the lungs of COVID-19 pneumonia patients in a systematic manner and compared them to cells from patients with pneumonia from other viruses or bacteria.

NGS also allowed Northwestern investigators to “map” gene expression in the lungs of COVID-19 patients onto those of fibrosis patients — a method that can help identify which patients are recovering well and which might require a lung transplant, such as the unprecedented life-saving lung transplant surgeries that have already been performed on patients with COVID-19 at Northwestern Memorial Hospital. This study was led by Ankit Bharat, MBBS, chief of Thoracic Surgery at Northwestern Medicine and director of the Lung Transplant program, and published in Science Translational Medicine (read more).
Northwestern investigators across many fields and specialties have emphasized how this fast and cost-effective technology has aided them in making discoveries, from examining the genetic components of Alzheimer’s disease to deploying clinical genetic screening and uncovering how genes influence cancer.
Probing Alzheimer’s disease
NGS has opened new doors in the study of Alzheimer’s disease, according to Robert Vassar, PhD, the Davee Professor of Alzheimer Research.
Recently, Vassar and collaborators took advantage of a database with whole-genome sequencing of 446 families with Alzheimer’s disease, searching for disease-associated variants of the gene coding for angiotensin-converting enzyme (ACE). Then, investigators created genetically modified mice with the newly discovered variants and discovered that those mice had neurodegeneration similar to that observed in brains with Alzheimer’s disease.

Going one step further, they treated the mice with ACE inhibitors and found the drugs prevented neurodegeneration and neuron death. These findings, published in Science Translational Medicine, helped further map out the disease-causing mechanisms underlying Alzheimer’s disease.
“NGS made possible the discovery of the ACE variant and the generation of the genetically modified mice that have provided important insight into the etiology of Alzheimer’s disease,” Vassar says. “As the cost of NGS goes down, it will continue to have an ever more significant impact on biomedical research.”
Providing genetically tailored clinical care
The rapid advance of NGS has made genetically tailored care increasingly viable, an evolution witnessed firsthand by Laura Rasmussen-Torvik, PhD, chief of Epidemiology in the Department of Preventive Medicine. Rasmussen-Torvik was a doctoral student in 2007 when the first genome-wide analysis platforms were made available to scientists, and she says it was a paradigm shift. One of the biggest leaps today, she says, is the ability to “examine genes across very large numbers of people.”

With the Electronic Medical Records and Genomics Network Phase III (eMERGE III) Project, that’s exactly what Rasmussen-Torvik and colleagues did. Over several years at 10 sites, the investigators screened more than 20,000 patients for damaging variants in 109 genes (looking for genes associated with cancer and cardiovascular disease) and found actionable gene variants in 3 percent of patients, according to a study published in Genetics in Medicine.
In the next phase of the study, according to McNally (who is also a principal investigator), the team will do the same for somewhere between five and 10 different common diseases. “We’ll recruit about 3,000 people and be able to tell them their genetic risk for getting one of these diseases,” she says.
This upcoming study, along with other implementation projects, suggests that clinical genetic screening is here to stay, according to Rasmussen-Torvik.
“It’s been a tremendously exciting 15 years to be in the field of genetic epidemiology, and I think we are going to see amazing discoveries and clinical uses in the next 10 years,” Rasmussen-Torvik says.
Attacking cancer
At Northwestern, some of the most important discoveries made possible by NGS have come in the fight against cancer. Designing precision-medicine cancer therapies is a cutting-edge application of genetics. The improved power and speed of NGS allows scientists to test thousands of candidate drugs that work against cancer on a fundamental biological level. The technology has helped Northwestern investigators, including Sarki Abdulkadir, MD, PhD, the John T. Grayhack, MD, Professor of Urological Research, crack the code for treating cancers caused by MYC.
MYC, a protein implicated in a wide variety of cancers, has an unorthodox structure that has bedeviled drug development for two decades. Abdulkadir and his collaborators used NGS to find non-toxic molecules that could bind to and block the protein, publishing their findings in Cancer Cell.
“NGS was instrumental in our ability to define the on-target versus off-target effects of various candidate MYC inhibitors, helping us to choose more specific, better tolerated compounds,” says Abdulkadir, who is also a professor of Pathology and principal investigator of the prostate cancer Specialized Programs of Research Excellence (SPORE) grant at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. “It’s put the molecular details of human cancer at our fingertips.”
Jaehyuk Choi, MD, PhD, the Ruth K. Freinkel, MD, Research Professor and an assistant professor of Dermatology and of Biochemistry and Molecular Genetics, sequenced genetic data from 29 patients with cutaneous gamma delta T-cell lymphoma in a study finding that the origin of cancer cells influences skin cancer prognosis, published in Nature Communications.
“We have a large number of these patients, but we didn’t have a framework to diagnose, stage or treat them,” says Choi. “This is our attempt to break through that clinical question by bringing personalized medicine to skin lymphomas.”
Other investigators, including Lifang Hou, MD, PhD, chief of Cancer Epidemiology and Prevention in the Department of Preventive Medicine and director of the Center for Global Oncology at the Institute for Global Health, delve into epigenetics (the mechanism that determines whether or not a gene is expressed), which is increasingly recognized as a vital part of oncogenesis. Hou developed a machine-learning approach that studies how one epigenetic mechanism, DNA methylation, impacts the risk of cancer through “junk” DNA, published in Clinical Epigenetics.
“Next-generation sequencing is becoming a fundamental tool in biomedical research,” Hou says. “The only limitation of next-generation sequencing technology is our imagination.”
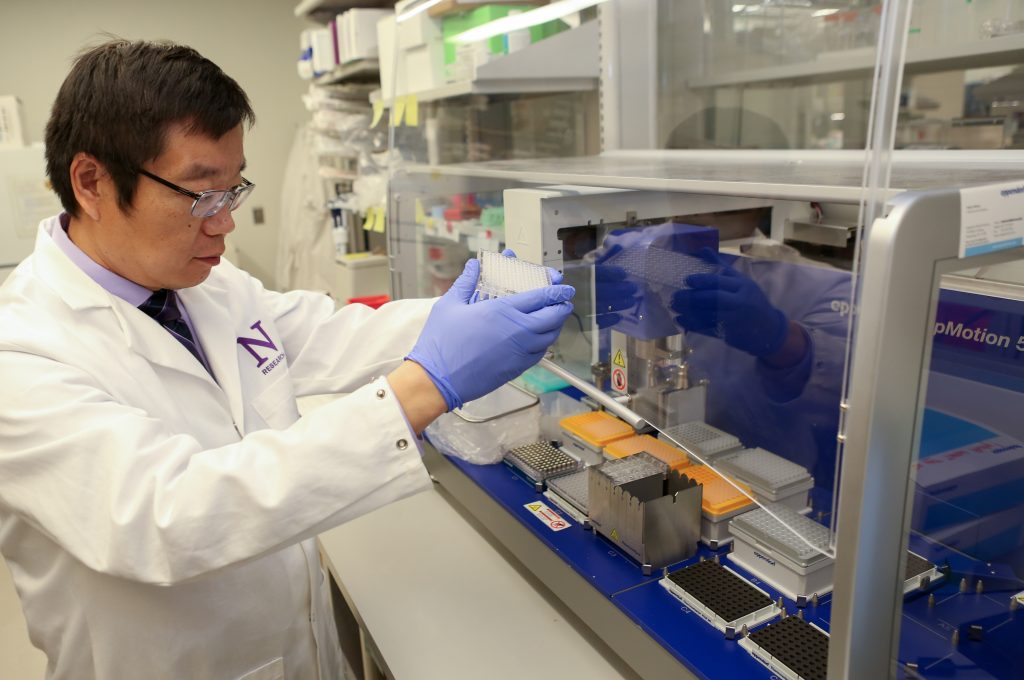
The unprecedented ability to rapidly read the genome, transcriptome, and epigenome has afforded us a holistic view of the DNA, RNA, and epigenetic codes in each of our cells, and thereby transformed the landscape of biomedical research.
Xinkun Wang, PhD
research associate professor of Biochemistry and Molecular Genetics, director of the NUSeq core